| Preston Hunt's Hodgkin's Disease Journal |
| In 2003, I was diagnosed with stage 3B Hodgkin's disease, a cancer of the lymphatic system. After 5 months of treatment under the Stanford V protocol (including 12 weeks of chemotherapy and 4 weeks of radiation therapy), I was officially declared in remission. I still receive regular check-ups, and my most recent physical exam and chest x-ray (April 2010) indicate that there is no evidence of cancer in my body! |
| First time here? Newest entries are on top to make it easier to find out the latest news. Scroll to the bottom of the page to read the story from the beginning. (You can also use the "Reverse Order" button below to read everything in normal order.) The Well Connected Health Series (PDF) has an outstanding overview article about Hodgkin's disease. I'm particularly proud of my daily pictures and journal, the bloodwork and stats, and the cost breakdown of my treatment. If you are interested in some different perspectives, you might enjoy Mike's story and Jill's story |
| Questions or comments? Send e-mail to [email protected] |
- 19 September 2013 -- Yay Stanford V!
-
One of my "Hodgkins Survivor Buddies", Jill, sent me this encouraging abstract: Risk of therapy-related secondary leukemia in Hodgkin lymphoma: the Stanford University experience over three generations of clinical trials.
It basically says that the lower doses of Stanford V have resulted in significantly lower rates of secondary cancers as a result of the treatment for Hodgkins. Go Stanford V! This is encouraging news after the results of the clinical trial I was in, which showed no advantage in effectiveness to Stanford V over ABVD.
- 6 April 2012 -- New oncologist, Dr. Ey
-
As I mentioned in a previous post, my long time oncologist (Kasra Karamlou) moved away from Portland last year. I chose Dr. Frederick Ey as my new oncologist.
I saw Dr. Ey today for the first time and he's awesome--I can see why he has such a good reputation. I gave him my full medical history and he gave me the usual annual cancer checkup.
Everything looks good. He said that there's really no need for me to continue with preventative chest x-rays or annual visits with him. I can check in with him if I'm worried about something, but otherwise my normal annual checkup is good enough. Sweet!
- 15 Aug 2011 -- Cancer humor
-
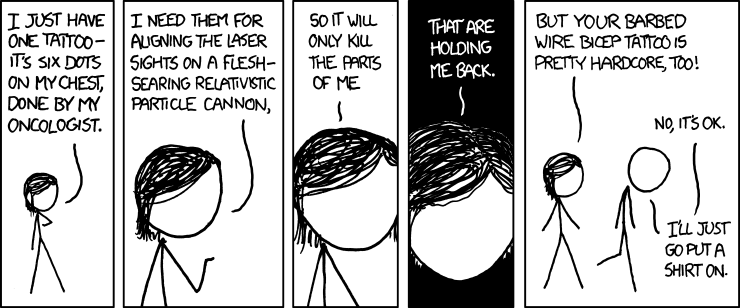
In preparation for my radiation treatment, I received five small tattoos that were used to align the radiation machine for my daily treatments.
So I really got a good chuckle from this xkcd cartoon, "Tattoo", when I came across it one day!
- 31 May 2011 -- I'm a dad!
-
Before I started my cancer treatment, I knew infertility was a possibility. I banked some sperm as a backup.
As the birth of our beautiful baby boy has proven, the cancer treatment didn't have any long-lasting effects on my reproductive system.
Welcome to the world, baby!

You can follow our adventures in parenthood at our baby blog.
- 1 May 2011 -- Need to find a new oncologist
-
I got a letter today with disappointing news. My doctor, Kasra Karamlou, is leaving the office where I've been going for treatment (Pacific Oncology). He's moving to Seattle.
Dr. Karamlou is a wonderful doctor. His departure is a big loss both for Portland and for me personally. He was there at the beginning of my cancer voyage, through the treatment, the cure, and the follow-on care. He always asks about Aimee and my parents, the latter whom he met only once I think! Visits with him are never rushed and he takes the time to thoroughly explain things and answer any questions in a thoroughly component yet empathetic manner.
Looks like I need to find a new oncologist for my care moving forward. I'm thinking of going with Gerry Segal at Northwest Cancer Specialists. He was one of the doctors that I went to for a second opinion when I was first diagnosed, and I recall liking him.
I'd gladly welcome any suggestions!
- 5 April 2011 -- Eighth year checkup
-
I saw Dr. Karamlou for my annual cancer checkup today. Physical exam and chest x-ray were normal; no news is good news!
Some more notable news that I have been eagerly awaiting is that the clinical trial that I was a part of (ECOG 2496) has ended. The trial's objective was to determine if the treatment that I received, called Stanford V, is better than the currently-accepted best treatment for Hodgkin's, known as ABVD.
The results are that, for patients with low-risk disease, there were no significant differences between Stanford V and ABVD. As a result, ABVD will remain the recommended treatment for most Hodgkin's patients. (My diagnosis was advanced, but low-risk, disease.)
This is not the result that that Stanford V researchers and I were hoping for. But at least it doesn't look like I am any worse off for having received Stanford V.
Here is a summary from one site I found (this presentation also has a nice summary, go to slide 54). I have removed portions of the excerpt that don't apply to my situation.
The Eastern Cooperative Oncology Group (ECOG) reported the results of their E2496 phase III trial comparing ABVD with Stanford V +/- radiation therapy in locally extensive and advanced Hodgkin lymphoma. This trial was designed to detect a 33% improvement in failure-free survival (FFS) with Stanford V compared to ABVD. Patients with locally extensive disease, stages I-IIA/B with bulky mediastinal disease (BMD), or advanced disease, stages III-IV, were randomized to 6-8 cycles of ABVD + 36 Gy for BMD versus 12 weeks of Stanford V + 36 Gy to sites >5 cm in diameter or for macroscopic splenic disease. In this trial, 812 patients were randomized. Forty percent of the patients with ABVD received radiation versus 73% of the Stanford V patients. There were no significant differences in ORR. Five-year OS was also not significantly different between the 2 treatment groups. Among the patients with advanced disease, FFS was similar for low-risk patients. The authors concluded that ABVD remains the standard of care, although Stanford V was considered acceptable therapy for certain lower risk patients. There were significant differences in the exposure to bleomycin and doxorubicin between the treatment regimens. Whether this will result in long term differences in adverse event profiles cannot be stated until further follow-up is achieved.
When you see n=812 for the overall trial (or n=408 for the Stanford V arm), I am one of the n's! - 18 November 2010 -- Thyroid, R.I.P.
-
My thyroid has conked out!
I went in for my annual checkup and my blood work showed that the thyroid stimulating hormone (TSH) in my body was high. TSH is a chemical message that the brain uses to tell the thyroid to produce more thyroid hormones (called T3 and T4). If TSH is high, it means that the thyroid is not working correctly.
This isn't a big surprise. The thyroid is very sensitive to radiation treatment and I always knew that I might run into thyroid problems at some point in life. The treatment is a simple, small, inexpensive synthetic thyroid pill that I have to take every morning for the rest of my life.
It is a little bit of a bummer. But it's mostly a good reminder that my body underwent some pretty serious treatment. I am keeping my fingers crossed that there aren't any more nasty side effects coming my way in the years to come!
- 5 February 2010 -- Seventh year checkup
-
Nothing noteworthy, everything is fine!
- 21 January 2009 -- Sixth year checkup
-
I'm down to once-a-year check-ups starting this year. I went in for my chest x-ray a few days ago and then for my physical check-up with Dr. Karamlou today. The usual stuff: radiology looks good, blood chemistry normal, body is looking good.
I asked about the clinical trial that I'm part of (ECOG-2496) and the only update is that the trial is still "collecting events". This means they are waiting for people to die so they can figure out which arm was better. That sounds morbid, but it's actually a good sign: both competing treatments are so good that it's tough to determine which is best.
- 5 August 2008 -- Fifth year checkup (part 2)
-
Not much to report out -- everything is fine!
I was clearing out some magazines, including issues of CURE, a cancer magazine. In flipping through one of the issues, I had dog-eared one of the pages on this article, which I recall really nailing how I felt at one point in my treatment: Dealing with the tyranny of positive thinking (and the sidebar, Losing one's right to complain).
CURE also published a good overview on Hodgkin's disease in their 2005 issue: Hodgkin's Disease: The Other Side.
- 19 February 2008 -- Fifth year checkup (part 1)
-
I went in to Pacific Oncology today for my twice yearly check-up. I don't recognize any of the people working there any more. I've been coming here so long that I'm starting to outlast the employees!
Dr. Karamlou reviewed the radiology report from my CT scan last week at St. Vincent's. Everything looked pretty good, except for a note at the bottom that said there is a small lesion on my hip that doesn't look cancerous but might be suspicious. The report recommended comparing the current scans with my previous scans to see how long it had been there.
This made me really mad. When I checked in for my scan, I specifically remembered giving St. Vincent's all of the info about my previous scans at Body Imaging. As part of the $2,000 they get for the scan and analysis, I would expect them to proactively obtain my previous scans and do the comparison. Dr. Karamlou said he would call them and ask them to do the comparison.
Otherwise, nothing out of the ordinary to report, except for some good news. After years of having depressed levels, my white blood cell count has finally returned to completely normal. I also mentioned that Dr. Doshi had gotten my cholesterol under control with pravastatin, which he seemed happy about.
UPDATE: Dr. Karamlou called and said that the radiologist compared my most recent scans with my previous scans. The suspicious lesion has been there for at least three years and is stable. Nothing to worry about!
- 14 February 2008 -- CT Scan
-
I went in today for what hopefully will be my last CT scan ever.
Up until now, I've been getting my CT scans at Body Imaging Radiology. They're great and have always been really good to me. Unfortunately, my insurance company (Cigna) decided to drop Body Imaging as an in-network provider last year. Cigna wants people to go to their hospitals to get scans. Obviously this is having a negative effect on Body Imaging's business. Body Imaging is suing to get access restored... I hope they win!
In the interim, Body Imaging has agreed to write off any amount that Cigna won't cover. Not wanting to mess with the whole situation, I decided to give the Cigna preferred provider (St. Vincent's hospital) a try.
Unfortunately, the experience at the hospital wasn't as good. It wasn't bad per-se, but definitely not as nice as Body Imaging. The hospital uses a different (worse tasting) contrast. The facility is very poorly laid out requiring lots of winding through corridors. Parking is nasty. Overall institutional feel.
I also was supposed to get a chest x-ray at the same time as my CT scan, but St. Vincent's didn't have the order. I ended up having to schedule a special trip a few weeks later to get the chest x-ray.
But the biggest disappointment, which I wouldn't find out until my follow-up with Dr. Karamlou a week later, was their slacker radiologists! Full details in the next post...
- 4 January 2008 -- Cholesterol follow-up
-
I've been taking my cholesterol medication for a couple of months now. I went back in today to The Dosh's office to see how well it was working. The type of medication I'm on (called a statin) can also cause liver damage in some people, so they did a liver test as well.
My total cholesterol is now 165, LDL 95, HDL 52, and triglycerides 89. Those statins really do work as advertised! My liver test came back fine as well. Double woo hoo!
After starting on Crestor back in November, I did a little web research to learn more about it. I figured that if I was going to be taking this drug for the rest of my life, a little due diligence would be a good idea. After reading Is Crestor dangerous and, if so, why? and also Dangers of Statin Drugs, I asked The Dosh if I could switch to pravastatin instead (which she agreed to).
My reasoning was as follows:
First, Crestor is an unproven drug. Pravastatin (also known by its non-generic trade name, Pravachol) has been around for a very long time and has amassed a large collection of data on its safety and efficacy.
Second, Crestor is new and thus still patented. This means it costs a lot. My insurance company thus charges me more as well. For a 30-day supply, my copay was $20 for Crestor, versus about $4 for pravastatin.
Third, high cholesterol takes many years to affect your health. There is plenty of time to take it slowly and start off with drugs like pravastatin which, while less effective than Crestor for some people, are time proven.
Fourth, having read the book The Truth About the Drug Companies: How They Deceive Us and What to Do About It, I know that it is quite common for pharmaceutical companies to release a stronger version of a drug that is not really more effective than an older drug, but has some new aspect that makes it patentable. And, unfortunately, the FDA testing does not really protect the public from this practice. (If you haven't read this book, read it!)
In any event, the good news is that pravastatin worked just fine in lowering my cholesterol and my liver is fine.
- 30 October 2007 -- Cholesterol check
-
I went to see my primary care physician, "The Dosh" (my nickname, her real name is Dr. Heena Doshi) on the advice from Dr. Karamlou that I get my cholesterol checked.
My total cholesterol came in at 231 (!), with an LDL of 149, HDL of 58, and triglycerides of 118. Not good.
The triglycerides and HDL are great, but the total cholesterol and LDL are abysmal. I asked The Dosh if I could lower my cholesterol without drugs by eating healthier, but she said I was too far gone.
She prescribed 5mg of Crestor daily. Crestor is the latest and greatest in cholesterol-lowering medications. We'll see how it goes!
- 21 August 2007 -- Fourth year checkup (part 2)
-
I went in for my second "year four" check-up today. My physical exam and complete blood count were fine, so I spent a while talking with Dr. Karamlou about recent developments in treating Hodgkin's.
The trial I am part of (ECOG2496, ABVD vs. Stanford V) is now closed to new participants, but it still may be a while before any results are published. The study needs to collect a minimum number of data points in order to be statistically significant.
We also talked about the importance of keeping my cholesterol level as low as possible. I'm at increased risk for heart disease as a result of the radiation I received to my chest as well as the chemotherapy. When I had my cholesterol checked earlier this year, I scored 196 or so. That level's borderline normal for most people, but for my situation, it would be better to be closer to 150. Guess I need to cut back on the donuts, cheese, and bratwurst :-(
I also had a chest x-ray later in the week. Nobody called with any urgent news, so I'll assume no news is good news. All in all, a great checkup. I'm looking forward to my next one in March which will be my last CT scan assuming all continues to go well.
- 6 March 2007 -- Fourth year checkup (part 1)
-
I'm in my fourth year since remission. This means that I only get CT scans once a year now and only have to get physical checkups twice a year. Woo hoo!
I had my most recent CT scan a couple of weeks ago (February 27th) and experienced the usual fears about the ever increasing amount of radiation I'm getting. Luckily I'm almost done: If all goes well, I should only ever have to have one more CT scan. Body Imaging has a new radiologist on their staff. He came out after the scan was done and peppered me with all sorts of specific questions which made it evident that he had done a thorough job of analyzing my scans.
When I met with Dr. Karamlou today, he said the CT scan results were perfect. My blood counts (white and red blood cells in particular) are also finally rebounding to their normal levels. Slightly depressed blood counts have been a minor side effect since I finished treatment.
All in all, everything's going great!
- 7 November 2006 -- Year 2.75 Check-up
-
Saw Karamlou today for my periodic checkup. My latest round of CT scans from a month ago were all fine. Thyroid level is normal. Bloodwork is mostly normal. My white blood cell count is still lower than average, but more than adequate for fighting off infections.
Starting next year, I drop down to one CT scan a year and two checkups a year. While I will be a little sad to lose the "security blanket" that frequent CT scans provide, I won't miss the substantial levels of radiation (perhaps as much as atomic bomb survivors?!) that they generate!
[Update April 2012: Here's another link on radiation exposure and cancer.]
- 7 June 2006 -- Year 2.25 Check-up
- Chest x-ray, standard bloodwork, and physical exam this visit. Everything still looks fine. I asked Karamlou to check my thyroid level and to call me if it was reading low. He never called, so it looks like my thyroid survived the radiation treatment (yay!). Pretty much good news all the way around for this visit!
- 3 March 2006 -- Year 2.00 Check-up
- 11th check-up since I finished treatment. Got another CT scan, which still shows no disease.
- 16 December 2005 -- Year 1.75 checkup
-
Thankfully, no surprises. Still doing great. Radiology report and bloodwork both came back "normal".
Life feels pretty much back to normal and I am back to working and playing hard, as this 2005 in review letter show!
The only bad news is that my chest x-ray original films are missing, probably lost forever. They got misplaced amidst all of the shuffling back and forth between offices. Not that big a deal since CT scans are far more accurate, but it makes me mad that we're still using old school films. Medical offices are slowly "going digital", hopefully we won't have to worry about lost records in the near future!
Even though the title of this post is "year 1.75 checkup", today actually marks the end of my second year of checkups. I'm 40% of the way through my "first 5 years". I had 6 checkups in my first year, 4 checkups in the second year, and will have 4 more in the coming third year.
- 13 September 2006 -- Year 1.50 Check-up
-
I went in for my 9th checkup since the end of treatment this week. I did my scheduled CT scan last week so that the results would be ready in time for my visit.
The CT scan place (Body Imaging) called me a few days after the scan, said their courier was too busy to take my films over to Karamlou's office, and if I wanted the films there in time for my appointment I would have to pick them up myself -- slackers! After picking up the films, I noticed that they had put a CD of my most recent 3 CT scans in the envelope. I immediately made a copy for myself, of course, and was pleasantly surprised when I popped it into my computer and it came with the necessary software to view the data. I spent the next hour or so examining the slices of my body and marvelling at it all. The bronchial tubes in particular were very interesting.
I also read the radiology report included with the films. For the first time, the report came right out and said that no active cancer was detected. Previous reports had all stopped just short of that absolute statement, preferring instead more conservative, lawyer-approved language ("...can't rule out...", "...may still be...", etc). Woo hoo!
With this prior knowledge, I wasn't expecting too many surprises from the actual visit with Karamlou. Except that it didn't end up being with Karamlou -- Oregon Hematology has a new doctor at that office, Anupama Kurup, and I saw her instead. To be honest, I didn't appreciate the bait and switch (this visit is costing $200, I wanna see the doctor I signed up for!), but I realize that the medical system depends on this sort of thing to train new doctors. And she did a fine job. But I was thankful that Karamlou grabbed me in the hallway on the way out for a quick hello.
This was my first visit to the office where my chemo nurse, Nancy, was gone. She accepted a job working with Carol over in clinical trials. So I was sad that I didn't get to see her, but happy for her that she will be doing new and exciting things.
- 14 June 2005 -- Year 1.25 Check-up
-
Went in for my year 1.25 checkup today with Karamlou, my 8th check-up since being cured. No problems to report. I am now officially in year two of my five-year check-up schedule. (Year 1 had check-ups every 2 months. Years 2 and 3 have check-ups every 3 months. And Years 4 and 5 have check-ups every 6 months. Then once a year after that for the rest of my life.)
As I'm writing this entry, I realize I never wrote about my one-year check-up back in March. Obviously everything was fine then, too. It's amazing how much things have returned back to normal in just a year: Unimportant quotidian concerns are already creeping back into my life, taking an increasingly larger share of my time and thoughts. Luckily, spring and summer are here at last and the explosion of life and activity is a good reminder to enjoy being alive.
Yet, despite the warm weather and long sunny days, the dark hand of cancer has me feeling a little melancholy: My neighbor had a recurrence of lung cancer that has spread to his brain (prognosis is not good). Another neighbor just found out that he has bladder cancer. (My condo building appears to be an unlucky place to live!) A friend at work found out that his colon cancer has come back and spread to his liver after 3 years of being in remission. A girl I knew from my young adult cancer survivor support group died of bone cancer. And two other Hodgkin's patients that I "met" on the Internet died recently as well. (One of them lived in Portland, and we exchanged some e-mails, but never met in person.)
- 14 February 2005 -- Fixed donation link
- Oops! After many reports from friends, I realized the donation link below was broken. It's fixed now below, or you can use this one.
- 13 February 2005 -- My mom's bicycle trip across America
-
In just a couple of weeks, my mom will be bicycling across America to raise money for cancer research and awareness!
As many people know, I bicycled 3400 miles across the USA in late 2003 and discovered just weeks after finishing that I had cancer.
My mom and her friend Lynda were inspired by both my bicycle trip and my cancer experience to pedal across the country themselves, raising money for good causes. They are taking a southern route from San Diego, California to Cocoa Beach, Florida. (My dad is going along as well, driving the support van.)If you are interested in tracking her progress, she has set up her own blog, which she will be updating from the road once she starts her trip. She also wrote a nice fundraising letter (PDF) describing her trip (and including a mini map of our route), and you can also check out her daily itinerary if you are interested in the details.
She is also raising money on behalf of the Lance Armstrong Foundation (which, as you may know, is a cancer charity). If you are interested in making a donation, it would definitely help motivate her in her journey, and would be appreciated by cancer patients and survivors everywhere (myself included). Note that 100% of your donation goes directly to LAF. Her trip is entirely self-funded.
- 19 January 2005 -- 10-month checkup
-
My first official cancer check-up of the new year and all is well and good! I did come down with a nasty cold that lingered around for a while, leading me to believe that my immune system is still not 100%. Or maybe the colds are just bad this year for everyone.
My next check-up in March will be the big 1-year check up.
- 23 November 2004 -- 8-month checkup
-
No news is good news!
- 14 November 2004, Sunday -- One year since chemo started; L'Hermitte's Sign gone; final cost breakdown; haiku
-
Almost exactly one year ago, I had just finished my first chemotherapy session. Sitting here now, healthy and happy, it's hard to believe that this whole thing even happened!
As far as my health goes, the only new news is that my L'Hermitte's Sign has gone away! It disappeared as suddenly as it appeared: I was in Italy on vacation a few weeks ago when I noticed that it was no longer happening.
I finally got around to tabulating up the final treatment cost: $77,633. See the cost breakdown page for details on where the money went, as well as the winner of the "guess how much it's going to cost" contest. It really surprised me at how cheap treatment ended up being.
Lastly, while I was cleaning out some computer folders, I found some haiku that Aimee and I wrote while I was going through treatment. We both think that we are the superior haiku writer. Please send me your vote for your favorite haiku so that we can settle our dispute once and for all :-)
Leaves fall, chemo drips
Sickness always follows; yet
The end brings rebirth
Drip, drip, drip. I watch
Bags of poisons slowly drop.
Presto will soon nap.
Discrimination
Is when you have cancer and
no one will massage.
It's like old growth woods
That is, Preston's hair. Strong. Tough.
Nurse Carol amazed
Men don't like lotion
Preston is no exception
Redneck, he became
Weeks after chemo
Weeks after radiation
Preston starts dancing - Tuesday, 15 September 2004 -- 6-month CT scan and check-up
-
I had my six-month CT scan a couple of weeks ago. It was a significant milestone since it's the first scan since I finished treatment, and the highest chance of relapse happens in the first year.
Today, I met with Dr. Karamlou, went over the CT scan results, and did the usual checkup per trial protocol.
Bottom line: The scan results look great! They aren't completely clear (and probably never will be) due to residual scar tissue, but this is consistent and expected for persons having had treatment for lymphoma. What's important is that there appears to be no active growth and all of the previous tumor sites are the same size or smaller than they were before.
I wanted to give a special "thank you!" to the people who noticed/remembered it was my 6-month treatment anniversary and called or e-mailed. It really meant a lot to hear from you.
Now that I am out and about in normal life again, it's amazing how many people I run into who say something to the effect of, "I heard about your cancer struggle, how are you doing, I've been thinking about you, etc." It's nice that people were thinking of me, but it would have been even better to have heard from them while I was going through treatment and needed the support the most. A simple phone call or (perhaps less awkward for some) e-mail is all it would have taken, less than one minute's effort. Ah well. [Update: Some people have asked me about this, commenting that I seem angry, so I want to add: I am NOT upset about this. Just remarking upon a phenomenon.]
- Sunday, 15 August 2004 -- First hair cut; hair changes from chemotherapy
-
Having grown accustomed to the clean look and low maintenance of short hair, I have wanted to cut my hair for some time now. But I have resisted before today because I wanted to see if the chemotherapy had altered the color or texture of my hair at all (as it is known to do).
I finally broke down today and shortened my hair down to about 1/2", but not before snapping a quick "status update" photo. It's hard to tell from the pictures, but my hair has definitely gotten darker, although it isn't any more curly or any less soft than it used to be. Only time will tell if it will ever return to its previous color, either from sun bleaching or as the chemo effects gradually wear off.
- Monday, 9 August 2004 -- Catching up
-
I've had several journal entries sitting around for a while, and I finally got around to posting them. The next three are all new, even though they are backdated for when they occurred.
- Monday, 26 July 2004 -- Medical appeal victory!
-
I received a letter from the medical appeal committee today -- I won my appeal to have the dental trays covered! A victory like this may seem like a small matter, but when you have been dealing with the medical insurance companies for as long as I have, it is quite delicious indeed when you win.
Although fluoride treatments are not normally covered by my medical plan, the reviewer noted correctly that, in my case, they were used to prevent major dental problems that sometimes arise after radiation treatment, including tooth decay and, in some horrible cases, the removal of the entire jaw.
I think this means that the medical plan at my company will be updated to include this as a covered service, so anybody else who finds themselves in a similar situation in the future won't have to go through an appeal.
- Thursday, 15 July 2004 -- Dental cleaning
-
Yesterday, I was washing my hands in the bathroom at work when I noticed that my teeth had this putty-like brown coating on them. The discoloring was mostly on the areas near the gums, but the fronts of many of the teeth were affected as well. I immediately freaked out, grabbed a toothbrush from my desk, and tried to brush it off with no apparent success.
I called my dentist and was able to move up my next dental cleaning to today, which was quite a relief. After a vigorous cleaning, including a significant amount of scraping with metal dental toolery, my teeth have now been returned to a state of semi-whiteness.
It turns out the staining was caused from the daily fluoride treatments that I have been giving myself to protect my teeth during and after radiation treatment. There are multiple types of fluoride available, but the cheapest and most common one (called "stannous fluoride", which coincidentally looks a lot like "stainous fluoride") causes the staining problem that happened to me.
Both my dentist and dental hygienist said that my teeth were looking great and that my saliva product was good. In light of this, I'm going to stop using the fluoride trays. They were a pain in the butt anyway.
- Wednesday, 14 July 2004 -- 4-month check-up
-
I went in for my four month check-up today. No news is good news!
The only real symptom I still have is the L'Hermitte's syndrome. Also, I never really seem to get a good night's sleep, but I suppose that particular problem afflicts millions of people.
The tiny bald patch at the top of my neck has finally started growing hair. This makes my hair recovery complete. Indeed, I would have to say that the hair recovery is too complete! In addition to having hair return in the normal ape-like places (side of hands, ears, nose), the bottom half of my jaw is growing hair about twice as dense as the rest of my face. This area was inside the radiation zone and was previously as hairless as could be. I'm hoping it returns to normal as it makes for a strange sight if I let my beard grow for a few days...
- Friday, 4 June 2004 -- Diagnosis confirmed; 3-month treatment anniversary
-
I saw my primary care physician today. Diagnosis confirmed: I have shingles.
If you don't know what shingles is, it's basically chickenpox that is able to break out again because the immune system is too weak to contain it (like all herpes viruses, chickenpox never goes away, it just lies dormant inside the body's nervous system waiting patiently to strike if the opportunity arises).
A weakened immune system often coincides with a period of great stess. The doctor asked me if I had changed anything in my life recently. I mentioned with a chuckle that I had gone back to work after being on disability for 6 months.
He said that I need to really take it easy for a while and prescribed a 10-day supply of Valtrex to help get rid of the shingles.
The story of getting in to see the doctor is a great example of one of the few benefits of having had cancer, as illustrated in my phone conversation with the office:
ME: Hi there... I have a weird rash on my chest and I think it might be shingles. Do you think I should see one of the doctors?
RECEPTIONIST: Yes, let me see when I can schedule you in. We're pretty busy until next week...
ME: Oh, I forgot to mention: I just got done with treatment for Hodgkin's disease... you know, chemotherapy, radiation. I'm not sure if that affects anything, but I thought I should mention it.
RECEPTIONIST: [Pause] Err... yeah, let me transfer you to the nurse.
[Short delay]
NURSE: Nurse So-and-so here.
ME: [Basically repeat what I already told the receptionist.]
NURSE: Oh, we definitely need to get you in here sometime today... umm, how does 11:20 look? [It was 9:00 when I made the call :-)]
Today was also my 3-month treatment anniversary.
- Thursday, 3 June 2004 -- Shingles!
-
I discovered a weird rash on my chest today. After digging around on the Internet a bit, Aimee and I are pretty sure it's shingles, which is common in Hodgkin's patients after treatment. One last parting gift from my bout with HD it would seem...
- Thursday, 20 May 2004 -- Health insurance rights seminar
-
Tonight I attended a free seminar hosted by the Leukemia & Lymphoma society on health insurance rights for cancer survivors.
The most interesting thing I learned about was OMIP, the Oregon Medical Insurance Pool.
OMIP is insurance of last resort, meaning that it is guaranteed medical coverage for all Oregonians. Oregon is one of only a dozen or so states that has a program like this, and I definitely sleep easier knowing it's there.
It is not free health care. The premiums are actually fairly steep, but if no other insurance company will cover you, you won't be complaining! Cancer patients that have been denied coverage from private insurance companies comprise the bulk of OMIP's membership.
According to the presenter, OMIP is not supported by any tax dollars, it has approximately 10,000 members right now, and the most expensive condition (on average) for all OMIP members is cancer.
- Monday, 31 May 2004 -- Memorial day weekend; first big hike
-
We had started to make big plans for Memorial Day weekend (long weekend in Seattle, trip to Oregon coast, etc.), but as the weekend drew near, we decided just to enjoy a lazy weekend around town.
In addition to a birthday party and a few BBQ's, Aimee, Beeman, and I climbed Dog Mountain, which is a substantial hike at 3,000 feet elevation gain and 7 miles round-trip to the summit.
I was huffing quite a bit and my heart was redlined the whole way, but I made it up without incident in about 2 hours.
See the rest of the Dog Mountain hike pictures or watch the three short video clips: one, two, three (videos require Quicktime to play properly).
- Sunday, 16 May 2004 -- L'Hermitte's Sign, 150 pounds, first MTB ride
-
I was sitting down this weekend and noticed a slight vibrating sensation that felt like it was coming from my chair. At first, I thought it was something in the building, but I eventually figured out that it was...
L'Hermitte's Sign!
Pronounced LUR-mets (I think), this is a condition where flexing your neck by looking down causes an electric shock-like sensation that extends down the spine (and sometimes into the limbs). It can be caused by many things, including multiple sclerosis, but in my case, it was caused by radiation treatment. Apparently the radiation treatments damage the myelin sheath surrounding the spinal cord and this causes the vibrating sensations. They typically show up several months after the radiation treatment and go away on their own after 6-12 months.
According to a study published in 1993, it occurred in 4 percent of patients who received >3000 cGy to at least 2cm of their spinal cord. Pretty rare, but it appears that I have it.
It's not really painful, just strange. An interesting thing about the shocks is that they are not continuous. After I look down and get the brief shock (which lasts a second or two), the sensation goes away completely. Looking down after the shock has been "used up" doesn't cause any further sensations until my spine "charges up" again (usually takes a few minutes). It also doesn't happen when I am lying down.
Other big developments this week:
I achieved my target weight of 150 pounds after a little dieting. The nurses at the radiation clinic chewed me out a bit for losing weight, but I'm going to maintain this weight until I lose the jelly belly that I've accumulated over the last 8 months of inactivity and then reassess what my ideal weight should be. (Incidentally, nothing else of interest happened at my radiation follow-up visit with Dr. Nautiyal last week.)
I also went mountain biking for the first time since starting treatment. It was pretty exhilarating but terrifying as well since I haven't ridden off-road in such a long time and I've kind of lost my mountain biking legs. I didn't break any speed records and was somewhat timid, but it felt great to be out shredding it up on the trails again!
- Friday, 7 May 2004 -- First week back at work; 2-month treatment anniversary
-
I finally returned to work this week after about six months off. It was really great to be working again, mainly because it means I'm healthy enough to return to normal life! Also, it feels good to be a productive member of society once more. And, of course, it was really good to see all of the friendly faces at work.
On the downside, it has been difficult getting used to the long work days after so long at home: The commute, meetings, running around the building, keeping my mind fully engaged all day... it all takes its toll. I find that I have enough energy to get through a day of work, but I'm so tired when I get home that I can't do anything but watch TV. This is a stark contrast to my usual summer routine of cramming in every possible activity in the incredibly long daylight hours of the northwest. For the time being, it seems that I have enough energy for either work or staying at home and doing an activity, but not both.
Today was also my two-month end-of-treatment anniversary. The whole thing is starting to feel like just a bad memory.
Symptoms update:
- Neuropathy: Fingers back to normal, all tingling gone!
- Hair: Most hair back to normal, although the radiation zone is still bare. My head hair in particular is growing in nice and thick. Still no indication yet on whether it has changed texture or color.
- Tinnitus: Slight ringing sound still present in my ears when it's very quiet (usually only at night right before falling asleep)
- Skin: Radiation burns are mostly faded, although my skin has become extremely sensitive recently. I think this is caused by all of the tiny skin hairs growing in, as well as cell regeneration.
- Itching: Gone.
My only real worry right now is that my teeth/saliva production will continue to be ok; I'm anxiously awaiting my next dentist visit. My throat is also very sensitive to spicy foods and I am prone to getting acid reflux problems (heart burn) if I'm not careful of what I eat. And, of course, in the back of my mind, I'm curious to see what becomes of my thyroid down the road.
- 27 April 2004 -- All clear!
-
The PET results are back: All clear!
I still need to confirm with the doc, but I believe this means I am officially either a complete responder (CR) or a clinical complete responder (CCR). Either way, cured!
- 26 April 2004 -- PET Scan
-
I had my PET scan at EPIC (East Portland Imaging Center) today. It was the most high-tech diagnostic procedure that I've received to-date and also one of the easiest.
I started out by signing two separate disclaimer forms promising to pay if the insurance doesn't come through. At $4,000 a pop, they seem a little nervous about people trying to run out on the bill.
Then the technician took me into a cozy room with a La-Z-Boy and injected me intravenously with the radioactive sugar solution (FDG - 18-fluorodeoxyglucose). I was expecting a large IV infusion, but the FDG came in a small syringe encased in metal shielding to minimize radiation exposure. The injection was quite cold but was over in a second or two. I reclined back in the La-Z-Boy and relaxed for 45 minutes so that the FDG could do its job. (Apparently the FDG injection alone costs $1000, making it my most expensive single injection to-date.)
I was then escorted across the hall to the PET/CT machine, which looked exactly the same as a CT machine to me: A mechanized gurney that slides back and forth through a big white plastic donut.
I whizzed once through the machine pretty quickly (CT scan) and then did it again much more slowly (PET scan). If I recall correctly, the scan was broken up into three separate parts, each of which took 10-15 minutes. I had originally worried about having to stay still for such a long time, but it didn't turn out to be a problem. I had brought some Ativan with me and taken a dose before the FDG injection to help me relax, so it was quite easy to let my mind drift in the dim room. At one point, I fell asleep and my hands, positioned above my head on a pillow, started to slip off.
It didn't seem like very long at all before the technician came back in and told me I was all done. She gave me some hot chocolate and a nutrigrain bar (I had been fasting and was pretty hungry) while I waited in the lobby. They like to verify that the scan was done correctly before letting you leave the office.
They said the results would be sent to my doctor within two days. Unlike the early days, when I was always super anxious to get my scan results, I am surprisingly calm and don't mind the delay.
- 21 April 2004 -- Delayed PET scan; cold
-
I was supposed to get my PET scan today, but I delayed it until next week because my cold turned out to be much, much worse than I had anticipated. I am only now starting to feel normal again. I'm not sure if the cold would have affected the scan at all, but since it measures metabolic activity, I didn't want to take any chances. Plus, you are supposed to lie still for up to 45 minutes, which I knew would be impossible if I were coughing every minute.
I had originally thought that I was having a hard time with the cold because my body was still recovering from everything that I've been through. I've since heard from many people that the current cold going around is particularly virulent, so maybe it was just a really nasty cold. Either way, I'm glad to be on the downhill side of this one!
- Friday, 9 April 2004 -- 1 month treatment anniversary; cold
-
It's been one month since my last radiation treatment. I would be celebrating, but I managed to pick up a cold somewhere during the last few days. Blecky. My last cold was way back in October, before being diagnosed, so I was overdue for one. It still doesn't make it any fun.
I must confess that I was a little excited about getting a cold since I wanted to compare it to going through chemotherapy. That excitement lasted about 2 minutes. Now I know that having a cold is way easier than going through chemo. And I'm ready for the cold to go away now :-)
The radiation burn on my neck has finally stopped hurting. The lumpy feeling in my throat is still there. My facial hair still looks freakish from where the radiation made it stop growing.
- Wednesday, 7 April 2004 -- CT Scan Results; Cured... most likely!; PET scan coming up
-
I called Dr. Karamlou and got the CT results: All tumors are gone except for the original large mass (7.5cm) in my chest, which has shrunk to 1.0cm. While the best news would be that all the tumors were gone completely, residual mediastinal mass is very common in HD patients. Often, if the original tumor is quite large, there will be permanent, benign scar-tissue that doesn't go away.
I guess this means I am in remission... almost! ;-)
For my peace of mind and to make sure that I am cured, Dr. Karamlou is going to schedule a PET scan for me in about 3 weeks. This site has a cool 3D PET scan image as well as some interesting case studies.
According to this "Blood" journal article, PET scans have excellent negative prognostic value:
However, in up to 64% of all HD cases, computed tomography (CT) or magnetic resonance imaging (MRI) show remaining tumor masses after completed treatment,3 although only a few of these patients will eventually relapse.4,5 These masses may represent fibrotic tissue or even an active Hodgkin tumor, but discrimination by CT is usually not possible.5 If the tumor is easily accessible, as an enlarged inguinal lymph node, the questionable lesion can be excised and histologically analyzed, whereas a mediastinal tumor can only be accessed by mediastinoscopy or open thoracic surgery. Mediastinoscopy is associated with a mortality risk of up to 0.5%6 and a high failure rate for a pathological diagnosis because of the relatively small amount of tissue that can be gained. Open thoracic surgery is an invasive procedure and thus not desirable for a potentially cured patient. Therefore, posttreatment mediastinal residues usually require follow-up CT scans at short time intervals. A delay in the diagnosis of progression or early relapse may result from this strategy and could mean a loss of precious time for salvage therapy.
[...]
The results of this trial clearly indicate that patients with a negative FDG PET result are unlikely to progress or relapse within a year or longer after therapy. The chance for remaining in remission in the first year after therapy is about 95%.
- Tuesday, 6 April 2004 -- Post-treatment CT Scan
-
Went to Body Imaging for my post-treatment CT scan today. Got to drink more of the yummy barium contrast and also got three more intravenous injections of the drug that makes my spine feel warm.
Things went pretty much as expected (I am an old pro at the CT scan now). Took about an hour for a chest x-ray and three CT scans (neck, chest, and abdomen/pelvis).
Unfortunately, the earliest I will get the results will be tomorrow. Let the waiting begin... I plan on taking 0.5mg Ativan to ensure a restful night's sleep and to keep the nightmares at bay. (I already took 1mg of Ativan last night to suppress any pre-scan jitters. Worked perfectly.)
- Sunday, 4 April 2004 -- Week 3 anniversary; nightmares
-
EOT+3 weeks and counting. Recovery still going well. I am sleeping much better and not taking as many naps, although I do have frequent and disturbing nightmares many nights. Two recent nightmares include one in which all of my teeth were coming loose and had to be extracted, and another in which I thought that there was something in my bed trying to get me (bug or snake, something along those lines). In the latter example, I freaked out and screamed, jumped out of bed, flicked on the lights... and finally realized that it was just a dream.
I've been biking up to Council Crest like a mad dog (4 times this week). My ascent time stands at 28m 08s right now. If memory serves, my best pre-diagnosis time was 20m 00s, so I have my work cut out for me. On my most recent ride, a dad and a little kid on a tandem blasted past me. It was very humbling. But at least I'm back out there!
My neck sunburn is finally beginning to ease up. A troubling new development is a funny tickle in my throat. My panicky side thinks that it's a mediastinal tumor growing again and pushing up against my trachea/esophagus. My reasoning side thinks that it's just another radiation side effect. Luckily I have a CT scan coming up in a few days.
- Thursday, 1 April 2004 -- Shaved-head tribute
-
I finally got around to making this tribute to my shaved head. Two games are available: "Where's Presto?" and "Identify the heads". How well can you do? :-)













- Sunday, 28 March 2004 -- Week 2 anniversary; Council Crest
-
Symptoms update: The itching has finally started to subside; hopefully this means that it was a side effect of the Oxycodone. The skin on my neck is still somewhat sore. I'm applying the aloe plentifully. I also started to lose my voice earlier in the week, but it wasn't painful and it's already started coming back.
Today Aimee and I bicycled to Council Crest (highest point in Portland) which is about 5 miles and 800 feet of elevation gain from my condo. I surprised myself by being able to make it without stopping since this is not an insignificant hill.
Council Crest holds a special significance to me since I have probably done it more than any other ride, and it was one of my training routes in preparation for the Ride Across America. In addition to getting me in shape, Council Crest helped me in my cross-country trip in another way: When faced with a large obstacle, Eric and I would convert it into more appealing "Council Crests": Instead of a 3000-foot elevation gain, we would say, "that's only 4 Council Crests!"
- Wednesday, 24 March 2004 -- Young adult cancer survivors support group
-
I attended a young adult cancer survivors support group last night. Now that I'm leaving the safety blanket of treatment, I figured I should at least try out some of the support group options available.
The meeting was pretty informal, mostly just people getting together and talking about anything and everything -- although, invariably, all roads led to cancer eventually. It was nice to have some fellow young people (defined as under 35 years old in the cancer community) since every other cancer-related activity I've been to seems dominated by the elderly.
There was a guy who had leukemia and a bone marrow transplant, a woman who also had leukemia and a BMT, a woman with a brain tumor, another woman currently being treated for breast cancer, a woman who had some sort of neck cancer, and me.
It was a good experience. I plan on heading back a few more times to give it an earnest chance.
- Tuesday, 23 March 2004 -- Post-radiation follow-up with Dr. Karamlou
-
I had my post-radiation follow-up visit with Dr. Karamlou today. We really won't know the answer to the big question (whether I am cured or not) until I get another set of CT scans, so we spent most of our time going through a long list of questions I've been compiling over the last month.
The short summary is that I can return to life as normal: Start taking vitamins and "lifestyle prescriptions" (Flonase, Allegra) again, eat all the sushi I want, exercise as hard as I want, etc. He thinks I should wait until May before heading back to work.
As for long-term side effects from my treatment: We'll check my thyroid level in 6-12 months to see if I will need to take synthetic thyroid replacement. My heart and lungs are probably ok if I haven't experienced any problems yet. My bone density was probably weakened by the prednisone, so I should start taking calcium and vitamin D supplements to counteract. As for infertility: Apparently there's no way to tell if the treatment damaged any reproductive organs. Looks like I'll be shelling out the $120/year cro-preservation maintenance fee down at the sperm bank :-(
Since I'm leaving the safety net of weekly office visits, I was worried about what I should do with any nagging little questions that come up in between my bimonthly office visits. Dr. Karamlou gave me his e-mail address so I can send him any quick questions that I might have. I thought that was pretty cool -- the way things should be done!
- Saturday, 20 March 2004 -- Back on the bike
-
I did my inaugural post-treatment bike ride today, the first time I've ridden since my diagnosis back in October. Aimee and Brian accompanied me for a leisurely ride down on the waterfront (about 8 miles total). The sun was out, the weather was nice, and it felt good to be back on the bike. I actually felt suprisingly good, but I forced myself to take things slowly and not overexert myself. The only time I allowed myself to "go for it" was on the return trip when I biked up the super-steep road to my condo.
I've been doing a little bedtime reading. The Journal of Clinical Oncology has a good article on The Optimal Treatment for Hodgkin's Disease. And there is an outstanding overview article about Hodgkin's disease from the Well Connected Health Series (PDF).
- Friday, 19 March 2004 -- One week anniversary
-
One week treatment anniversary today!
My throat is feeling much better. It is still a little sore, but at least I can swallow now without the food torturing me on its journey down my esophagus.
My neck is still pretty sunburned. I constant apply aloe vera, which provides a temporary relief, but my skin has an insatiable appetite and just sucks it down.
I have been off of the oxycodone for several days now. I am still moderately itchy, but I am hopeful that it was a narcotic side effect and that the itching will stop in a day or two.
My energy level is continuing on its way up. I went to the zoo today with Andrew and walked about 3.6 miles total, my biggest exercise day to-date.
Aimee commented the other day that my head finally doesn't have the shaved look any more. My moustache area is growing at a healthy clip too, but the rest of my facial hair is still a little sluggish (as is the hair on the rest of my body).
I just updated my medical costs if you have been following along (see right hand side bar).
- Monday, 15 March 2004 -- First day off
-
My first day without treatment; the first day of the rest of my life!
Throat still hurts. Skin still sunburned. Starting to lose my voice. Slept in until 12:30!
Now that treatment is over, I'm going to scale back the daily photos to once per week. It was starting to become a chore anyway.
- Friday, 12 March 2004 -- DONE!!
-
Today brought my final radiation treatment... and the end of my treatment! People have been asking me if I am planning a big party to celebrate, but in reality I am too exhausted to do much celebrating. I am just glad to be done. I plan on celebrating in a week or two when I can enjoy it.
The technicians and nurses all congratulated me on being done and reminded me to stop by the treatment room and say "hi" when I come back for check-ups. I said farewell to all of my radiation buddies in the waiting room as well. We all started to say, "see you later," but ended up with "it's been nice knowing you, but let's hope we never have to meet under these circumstances again!"
One guy in the waiting room was jealous that I was done, saying that he had four more weeks to go. But the time truly has flown by very quickly and I told him that he would be done before he knew it. The daily appointments were somewhat relentless, back-to-back with only the weekends off (just like a full-time job!), but one benefit of such frequent treatments is that it's all over quickly.
Dr. Nautiyal was out of the office for my final office visit, but he called me last night and wished me good luck, said it's been a pleasure treating me, etc. Yet another example of his considerate nature.
I went home and promptly fell into a deep slumber for three hours. I am certainly glad that the treatments are over -- I don't think that my body could have taken much more of this. My skin is totally sunburned, my throat is sore, and the itch from the oxycodone is wearing me down.
Unfortunately, even though my mind thinks I'm done, my body hasn't gotten the news. The sore throat and sunburn won't be gone for a few weeks (indeed, they may get worse before they get better), and it may be months before the fatigue goes away.
I was surprised at how few people congratulated me on being done. Don't worry, I'm not feeling sorry for myself or anything, but this is such a big milestone in my mind that I was sort of expecting the phone to be ringing off the hook. I hear from other cancer survivors that this is the norm, however, especially on subsequent check-ups (6 month, 1-year, 5-year, etc.), which are huge anniversaries to cancer survivors but are hard for friends and family to remember or realize the significance.
- Wednesday, 10 March 2004 -- Itching mystery solved (?)
-
Dr. Karamlou says that the oxycodone is the culprit behind my itching. He seems very confident that it is not a relapse of Hodgkin's disease. I am going to discontinue using it tonight and we'll see if the itching goes away.
I had a huge list of questions queued up to ask him, but since we are meeting again in a week and a half, I decided to postpone asking them. He did ask me when I was planning on returning to work. I said 2 weeks after treatment ends, to which he said, "No, no no... you need at least 4 weeks to recover. You can try going back sooner, but you'll be exhausted."
So it looks like I'll be heading back to work around the second week of April.
- Tuesday, 9 March 2004 -- Hair falling out again; still itching
-
The hair on my neck and in the middle of my chest has fallen out as a result of the radiation treatments. Between the missing hair and the red skin, it's easy to see exactly which parts of my body are getting zapped.
My throat is still feeling fine, I'm still sleeping a ton, and my skin still itches all over. I'm meeting with Dr. Karamlou tomorrow to discuss the itch.
Otherwise, only 3 treatments left until I'm done with treatment forever! Woo hoo!
- Friday, 5 March 2004 -- End of week 3 (75% done)
-
I am 75% done with treatment! As the Chinese proverb says, the journey of a thousand miles begins with a single step. Still, I can't believe how quickly the time has passed. Only one week to go... I'm pretty excited about finally being done!
My throat is starting to feel really good and isn't giving me much pain at all anymore. I'm not sure why, but apparently my throat has either adjusted to the radiation or has stopped complaining.
One new symptom is that a thick filmy layer of sludge has formed on my tongue. It's pretty nasty stuff. I scrape it off with a toothbrush a few times a day, but I can tell that it won't go away until treatment is over.
I met with Dr. Nautiyal after treatment for my usual Friday check up. There wasn't much to talk about since I haven't really had any problems this week. Dr. Nautiyal remarked that I was doing really well. He also noted that week 3 is usually the toughest for most people, so hopefully my final week will be smooth sailing.
By biggest worry lately has been itchiness all over my body. Itchy skin is one of the symptoms of Hodgkin's disease (along with weight loss, night sweats, fatigue, and fever), so sometimes I start to freak out and worry that I might be relapsing! Hopefully, there may be another explanation: All the hair that fell out during chemotherapy is starting to grow back in all over my body and I think that may be causing the itching. I'm also assuming that being under stress might be causing some itching (just like it caused canker sores to appear in my mouth).
Still, I can't wait to talk about it with Dr. Karamlou at our next visit... and to have a CT or PET scan confirm that nothing's wrong!
- Tuesday, 2 March 2004 -- Throat soreness; sunburned skin
-
My throat is starting to feel very sore, but strangely the lump-in-the-throat feeling is gone! The overall result is that I am doing much better. I can deal with a sore throat but that lump feeling was intolerable!
My neck is getting very red and dry and looks sunburned. It also feels pretty sore. I am applying a lot of aloe vera to try to keep it from getting any worse.
I have added ativan to my nightly dose of oxycodone and the result is a really good night's sleep! Still, I am pretty sluggish throughout the day and have to take multiple naps. I usually catch an hour or two after I get back from treatment and then grab a second nap just before sunset.
Even though I am entirely unmotivated to do so, I force myself to take a walk downtown every day. I usually walk between 1.5 and 2 miles round trip each day.
All in all, despite all my complaining, the radiation therapy has been much more tolerable than chemotherapy was. The old saying, "my worst day of xxx is better than my best day of yyy ever was" comes to mind.
- Sunday, 29 February 2004 -- Oxycodone works!
-
The oxycodone works great! My throat gave me a lot less trouble the last two nights and I was finally able to get a decent night's sleep. The humidifier also helps a bit, but it's pretty loud, so I probably won't keep using it.
During the day, my throat is still giving me quite a bit of trouble. I have tried using the oncology mouthwash, but it doesn't really work that well for my throat. The lidocaine numbs my lips and mouth really well, but when I swallow it, it blasts right past the part of my throat where I need the help the most. As a result, I'm still having a lot of trouble eating and drinking.
I was hoping that having the weekend off from treatment would make me feel better, but it hasn't seemed to have made much of a difference. Unlike chemotherapy, where each day off relieves more and more symptoms, radiation is much more of a cumulative effect where the symptoms slowly get worse as time goes on.
I am pretty nervous going into week three tomorrow since I have read that it is when most patients start to experience really bad symptoms.
- Friday, 27 February 2004 -- End of week 2 (50% done); canker sores
-
It's hard to believe that the end of week 2 is finally here!
Overall, I'm hanging in there pretty well. I was pretty panicked at the beginning of the week because I worried that my throat would become unbearable by the end of the week, but luckily it has been in a holding pattern. My throat only hurts when I swallow, which means it's not that big a deal during most of the day.
Eating and drinking suck however. I am having trouble staying hydrated and keeping weight on. I feel like one of those stomach-bypass patients in that I can only eat teensy bites of food at a time -- and I have to chew each piece to death, otherwise it wreaks havoc on the way down my esophagus.
Nights are pretty bad. When I lay down, it feels like there is a bump in my throat. And there is some sort of post-nasal drip that makes me wake up every few minutes to clear my throat. The end result is that I am exhausted all the time. I feel quite weak/fatigued physically as well.
The skin on the back and sides of my neck has broken out in a rash. It gets pretty itchy at times, and also aches a bit, especially when clothes rub against the skin. And it's started to peel like it's been sunburned.
Lastly, a few canker sores appeared underneath my tongue yesterday. They aren't painful and they seem to come and go. Just another symptom to deal with. I asked the nurses about the canker sores, and they said that they aren't caused by the radiation, but are most likely caused by stress.
I am feeling pretty stressed out. Most notably, I have nightmares every night. Mostly fear of relapse, but also some radiation treatment related fears, such as losing all of my teeth (Dr. Nautiyal assures me that this is not going to happen).
One waking fear that I have is related to constantly being itchy all over my body. Itchiness is one of the symptoms of Hodgkin's disease, so whenever I get an itch, there's always a little voice in the back of my head that wonders if it's the disease coming back. I think the itchiness may be caused by my hair growing back in all over my body.
Dr. Nautiyal recommended taking oxycodone before going to bed to help with my throat discomfort. He said that placing a humidifier next to the bed may help with my throat. And also that many patients find sleeping on the couch more comfortable during treatment. I plan on giving some or all of these suggestions a try this weekend!
- Thursday, 26 February 2004 -- Waiting room; radiation
-
Aimee and I are getting to know the other patients in the waiting room, which makes the daily trips a little more fun. Seeing guests accompany the patients is much more common here than with the chemotherapy. It turns out that they don't run as tight a ship here as I initially thought, so there is plenty of time for talking while we are all waiting.
There's an 80-year-old guy (patient) and his daughter (guest); I don't know what he is being treated for, but he has a lot of life in him! The daughter is intense and firmly believes in the healing powers of naturopathic medicine.
There's a 30-something guy being treated for prostate cancer. His treatment lasts 10 weeks. His eyes are always half-closed and he moves and talks languidly as if he is in a lot of pain. Despite this, he's very gregarious and talkative.
Lastly, there's a young 20-something guy being treated for testicular cancer (his dad is always there too). His cancer was detected early enough that it was removed surgically (no need for chemotherapy). His treatment, like mine, is mostly preventative to make sure that all of the cancer is gone.
I'm also getting a bit more chatty with the nurses and technicians. One of them asked me about my shaved head, since they had seen me a while back with a bit of hair. This led to a discussion about chemotherapy and which drugs I had been on. They all seemed impressed by the sheer number (seven) of drugs that I was on. Most of the patients they see are old and can't handle more than one or two drugs at once. On a related note, there aren't many young people getting treated. The technicians sometimes have trouble telling us young people apart since we all look the same compared with the majority of their patients :-)
Every so often, a technician-in-training is present in the treatment room. I've seen one guy in particular two or three times. At first, he was just observing, but lately, they have let him help with my alignment or in adjusting the radiation machine (all under supervision, of course!).
- Tuesday, 24 February 2004 -- Throat discomfort; sleeping problems
-
After a week without incident, my first side effect has arrived with a vengeance! My throat started to feel quite uncomfortable late yesterday: I had a little trouble swallowing, but mostly it felt like something was caught in my throat. The discomfort got worse all night, resulting in my getting very little sleep. I woke up every few minutes due to lots of throat clearing and hacking.
One of the benefits of daily treatment is that I don't need to wait long to talk to the doctor or nurses about any problems. I spoke with Dr. Nautiyal for a few minutes about the throat discomfort. He said that this is usually the first symptom that patients receiving neck treatment get. I was worried that it had occurred so soon (after only 6 treatments), but he said that it was not unexpected since my treatment area envelops so much of my upper chest.
He gave me a prescription for "oncology mouthwash", which is a mixture of lidocaine, benadryl, and one other ingredient. It is supposed to numb the mouth and throat for short periods of time (especially useful before meals). I filled the prescription but didn't end up using any yet since I am still able to get food and liquids down with lots of chewing.
Dr. Nautiyal reassured me that if my symptoms got much worse by the end of the week, that he would reduce my daily radiation dose a bit. This would help alleviate some of the symptoms at the expense of extending the length of the treatment.
- Friday, 20 February 2004 -- End of radiation week 1 (25% done); Dr. Nautiyal meeting
-
I'm 25% done with my radiation therapy as of today.
In addition to my daily treatment, I have regularly scheduled meetings with Dr. Nautiyal each Friday. It was a pretty quick meeting this week since I really didn't have any symptoms to report. A surgeon was shadowing Dr. Nautiyal; he obviously wasn't a new doctor in training. I think he was doing some cross-training, keeping up-to-date on other disciplines, that sort of thing.
Dr. Nautiyal surprised me last night with a call at home. He wanted to tell me that he had finally heard back from the radiation folks at Stanford. They are supposed to approve the radiation plans for each clinical trial patient, but they had been ignoring repeated calls from him up until now. They gave a thumbs up for everything Dr. Nautiyal has planned for me, which is a good thing since I am already a week into it! Anyway, Dr. Nautiyal knew that I was anxious to hear what Stanford had to say and I appreciate that he stayed late at work (6:45pm) to call and let me know. He is a very caring, considerate, and hard working doctor!
My only real "symptom" to speak of is psychological: I worry a lot about the long-term side affects of radiation. To help assuage my fears, Dr. Nautiyal whipped out my treatment notebook, and showed me some of my various simulation reports. One of the reports show how much radiation various parts of my body are going to get (lymph nodes, spinal cord, parotids, etc.). I was really impressed at how he was able to deliver 100% of the radiation to the lymph nodes while delivering much less radiation to all of the other organs in the area (a few places get 50%, but most areas get much much less).
I am looking forward to having the weekend off from treatment. Even though the treatments are short and I haven't had any symptoms, the daily treatments feel a bit relentless at times.
- Thursday, 19 February 2004 -- Radiation treatment #4
-
They run a tight ship down in the radiation department -- things pretty much run right on time. The typical visit for treatment takes about 10 minutes total from the time we enter until the time we leave.
After arriving at the office, we walk right past the receptionist's desk (no check-in or copays, woo hoo!) and sit down in the waiting area, which also doubles as a changing room. There are separate rooms for men and women, but there are always plenty of women hanging out in the men's room. The room isn't crowded; usually just the person who went before me and the person going after me. Many people, including myself, don't change at all, since the radiation is to our upper bodies and we will have to take off anything covering our chest anyway.
When it's my turn, Michelle (radiation technician) comes down to get me and escorts me back to the treatment room. In the treatment room, I take off my shirt and lie down on my customized styrofoam bed. Michelle and Nancy then spend a few minutes adjusting both the bed and me. Once I am aligned, my powers of observation are more limited since I am too petrified to even move my eyes around for fear that I'll accidentally move my head as well, causing the wrong body parts to get zapped.
After my body is perfectly aligned, somebody slides a plastic tray into a holster directly below the radiation aperture. The plastic tray has several 10cm thick lead blocks screwed to it. The lead blocks were custom sculpted based on computer models to shield as much of my body as possible from the radiation. On my tray, there are two blocks that shield the sides of my chest (lungs, etc.) and another block that shields the right side of my neck.
Once the tray is secured, Michelle will call out "110", which I originally thought was some code word for "ready to go", but I later learned is the distance of the treatment bed from the radiation aperture. Even if it isn't a code word, it does seem to act as a transitional phrase, as the next step is always the treatment.
The treatment is given in two steps, first to the top of my body, and then to the bottom. For each treatment, everybody leaves the room and the door is closed. Out of the corner of my eye, a computer monitor starts flashing something (probably a big warning message like "GET OUT OF ROOM NOW!"), and that is my only indication that treatment is about to begin.
The treatment itself lasts about 30 seconds and is not painful. The only unpleasant part of the treatment is a weird odor that I sense whenever I exhale. It only happens when the radiation beam is "on", and the odor goes away as soon as treatment is over. I asked the technicians and the nurses about this phenomenon, and they looked at me like I was crazy. They said that I was the first person to ever mention this to them. I later discovered from a Hodgkin's mailing list on the Internet that many people have had this response, although the exact cause is unknown. The prevailing conventional wisdom is that the radiation changes some of the oxygen (O2) in my lungs to ozone (O3) and that is what I am smelling. (I later asked Dr. Nautiyal about this, and he said that it wasn't ozone... and that there is no medical explanation for it.)
As a result of the odor, I try to exhale as little as possible during treatment. Holding my breath the whole time is a bit uncomfortable, so I have found that doing two complete (but s-l-o-w) breathing cycles is a good compromise.
After the top side is done, somebody comes back into the room to swap out the shielding tray. The big arm holding the radiation aperture rotates down under the bed as the bed simultaneously raises up in the air. It's a pretty impressive feat of machinery in motion, especially when you consider that the machine has to align itself perfectly after each movement.
Because the radiation beams are attenuated differently when they enter the body on the bottom, a different shielding tray is used. The technician swaps out the second tray, usually says something like "here's the second part", leaves the room, and the treatment described above is repeated.
Throughout the whole treatment, I am supposed to lie perfectly still with my hands above my head, my chin thrust up into the air, and my head cocked slightly so. My number one fear throughout the treatment is that I will move slightly causing the wrong areas to be irradiated.
The post-treatment routine is pretty unceremonious. I put my shirt back on, bid adieu to the technicians and leave, but by this time, they are already busy preparing the machine for the next patient. With the tight schedule, there isn't much time for chit chat or bonding with the technicians. Not that I blame them. They have tons of patients to see. Patients also go every day, so a few minutes of chit chat every visit would multipy into a significant amount of time!
Another scary observation is how many treatments they give in a day: 10 or 15-minute slots all day long, each one representing a cancer patient. That's a lot of cancer patients.
- Monday, 16 February 2004 -- Radiation treatment #1
-
I had my first radiation treatment today. Because this is my first visit, they did some additional diagnostic and quality control procedures, which stretched my total time in the office to about an hour. All of my future visits will be treatment only, which will just take a few minutes. I'll focus on the unique aspects from the first day right now and cover a typical visit in a future journal entry.
The radiation technicians, Michelle and Nancy, introduced themselves and then got to work fitting me to the custom styrofoam mold bed that was made a couple of weeks earlier. The radiation machine is just a sled with a giant arm that hangs over your body. There are a bunch of alignment lasers that shoot all over the place as well. The room itself has no windows and a thick, shielded door. The styrofoam mold beds for all of the other patients hang on the back wall. An elaborate shelf system holds the custom built lead shielding plates for each patient.
Michelle and Nancy spent quite a bit of time tugging on the styrofoam mold bed until it was positioned perfectly. They then micro-adjusted my body (a push on the shoulder here, a nudge of the chin there) until I was perfectly aligned as well. Using a Sharpie pen, Michelle marked off the exact area on my body that would be radiated. Of my seven tattoos, I think the one on my chin and the one near my port were not usable anymore for various reasons. Nancy drew a small line just below my left jaw with an alcohol-resistant marker. This line will ensure that my head is tilted correctly on future visits. They will "touch up" the line every day throughout my treatment. They said that they use the marker to avoid having to give patients additional tattoos, something I definitely appreciate!
After the alignment and marking was complete, three or four sets of diagnostic x-rays were made. Each set comprised two exposures. The first exposure was just like any other x-ray I've had; on the second one, I noticed a blue light and a funny odor while the radiation beam was on. In between each set of x-rays, I had to wait on the bed, lying perfectly still and trying not to move at all. The whole time, my head was cocked at a slight angle and my arms were hanging over my head. After almost 30 minutes of this, my arms and head started to feel pretty sore. At one point, my butt fell asleep as well.
Once the x-rays were complete and verified, Dr. Nautiyal came into the room, checked everything, and gave his final approval. While he was there, he told me that my neck extension was very good and that he was able to spare all of my right parotid and most of my left parotid from radiation. Damage to the parotids is the primary cause of dry mouth, so this was welcome news.
The treatment itself was quick and painless (more on this later). Afterwards, we set the regular appointment time at 8am (yawn!) and left for home.
While I didn't experience any nausea or pain, the first treatment definitely knocked some of the wind out of my sails. I had been feeling quite good over the past few weeks, but it felt as if the first radiation treatment had erased all of the gains I had made since the end of chemo. Upon returning home, I didn't really feel like eating or drinking anything, and I took a long nap in the afternoon.
- Sunday, 15 February 2004 -- Shaving my head
-
Aimee has been threatening to start calling me "The Donald", so I decided to throw in the towel and shave off my remaining hair. It's ironic that I didn't have to do this until two weeks after my chemotherapy ended, but that's life in the Wonderful World of ChemoTM.
I really had no choice as my head has continued to drop hundreds of hairs a day. It was a mess up there. A large "U" shaped bald spot had formed on the part of my head that rubs against my pillow. It was this spot in particular that convinced me to shave all of my hair off.
Now I get to see my head in the "chia pet" stage when my hair does finally grow back. This is also the ideal time to experiment and see exactly how I look with a shaved head! At the very least, I'm looking forward to not having to shampoo or worry about styling my hair.
Aimee and I had set aside Sunday evening as head shaving time, which happened to coincide with a last-minute visit from Brian and Grace. Brian volunteered to do the shaving honors. I think he did a pretty good job!
See the head shaving pictures
- Thursday, 12 February 2004 -- Week off; enjoying life
-
With no doctor's visits to attend, treatments to endure, or medication to take, this has been a truly wonderful "week off". I am definitely getting stronger and more energetic every day.
My week off has coincided with a break from the normal rainy deluge in Portland. It has been absolutely gorgeous all week. I have been taking long walks (almost 4 miles total today) downtown, simply enjoying the warmth of the winter sunshine on my face, the call of the birds at my ears, the gentle tug of the occasional breeze on my hair, the beauty of both nature and man's accomplishments in my eyes.
It feels so good to be able to walk around and not feel weak, sick, or nauseated! As my head bobs to happy tunes on my iPod, I observe stressed out people all around me scurrying about their lives. I want to stop and shake them and make them slow down and embrace and enjoy their healthy lives. But I realize the futility of such desires. I too was a scurrier not so long ago.
In parting, I leave you with two reading assignments: Three Days to See by Helen Keller and Gordon the Guided Missile. Determining what's truly important in life and adjusting your life accordingly is a daunting task. Let me know if you figure out how to do it :-)
- Monday, 10 February 2004 -- First week after chemotherapy
-
If you measure from the date of my last chemotherapy treatment, I have been done for two weeks. If you measure from the last day of the chemotherapy cycle, I have been done for one week. Either way, I am feeling much better. I have zero nausea, my energy level is picking up, and my appetite has pretty much returned to normal.
My sleep pattern is slowly returning to normal as well: I was getting about four hours of sleep during chemotherapy; I estimate that I'm getting around six now. I toss and turn a lot, however, and always get up once to go to the bathroom, so the sleep is not as restful as it could be. I am also having quite a few nightmares, mostly a scene in the doctor's office where a huge lymph node/tumor is growing somewhere on my body (like my ankle) and I am freaking out about it to my doctor.
My hair continues to fall. I had expected the hair loss rate to slow down considerably after chemo, but it is still going at a pretty good rate. Every few days, I am still tempted to go ahead and shave it off as it is looking pretty bad (much worse than Donald Trump's hair, and I used to think that his was the worst!). There is a thin veneer of hair that hangs like scaffolding over my head, and then pure baldness underneath. Hopefully it looks no worse than any other man who is losing his hair.
Here's a deforestation report for the rest of my body:
- Eyebrows: Thinning, but not too bad.
- Beard: Soft peach fuzz hair. I only need to shave every other week.
- Chest: About 75% gone.
- Armpits: About 75% gone.
- Private parts: About 95% gone.
- Everywhere else (arm, leg, toes, etc.): Pretty much unaffected.
My fingertips are still numb, although my pinkies are stating to return to normal.
My legs, and especially my knees, ache a lot. I am hoping that these are mere artifacts of my sedentary lifestyle and not something more serious. I have seen some complaints about bone mass and muscle loss caused by Prednisone on some of the Hodgkin's support groups on the Internet. However, I have not been able to substantiate these claims with any reputable sources on the net; I plan on asking Dr. Karamlou about it next time I see him.
- Friday, 6 February 2004 -- Portacath removal surgery
-
I was originally scheduled to have my portacath removed on 23 February, but Dr. Nautiyal didn't want me to have any surgery once my radiation starts on 16 February. Dr. Khaki's office was able to move up my surgery to today, although I had to go really late in the afternoon (2:00 check-in for 4:00 surgery). Sometimes this makes me nervous as I worry that the doctors and nurses will be tired after a long day of work, but I suppose it's nothing compared to 120-hour weeks they put in during residency. Also, you are not supposed to eat or drink ANYTHING (including water) starting 12 hours before the operation. Being dehydrated and hungry was not a pleasant way to spend my morning.
My trusty portacath has served me well. I was a little uneasy about getting it taken out since having it was a safety blanket of sorts (what if I relapse and I need it again?). In the end, I think that the psychological benefit from having it out far outweighs the small chance of relapse. In addition, although generally quite safe, portacaths are foreign bodies and can form blood clots or have other deleterious effects on your body.I estimate that the total roundtrip cost of the portacath will be about $7000. I used it for 15 chemo treatments, which comes to $470 per use. So it was a bit expensive and a hassle to put in and take out, but I saved the veins in my arm from a substantial amount of abuse. All in all, I'm glad I got it.
The surgery was pretty much the same as my previous two, except that I notice more and more stuff with each successive visit. The only things worth commenting on are:The first nurse who tried to set up my IV did a terrible job. She failed twice before handing off the task to someone else. Because the best two choices were already ruined, she put the IV into a vein on my hand, which was a first for me! A few days later, huge bruises appeared from all of the leaked blood at the two failed IV sites.
I learned that you can request a specific anesthesiologist if you call the OR ahead of time (although this may require some schedule flexibility). Since there was such a difference between my first two anesthesiologists, I was hoping that this time would be more like Dr. Wong and less like Dr. WhoeverItWas. Dr. Robinson turned out to be wonderful and I would highly recommend her. She has an excellent bedside manner and expertly administered the drugs so that I hardly felt groggy at all when I came to. In Dr. WhoeverItWas's defense, he had to put me out for a much longer and more involved operation.
The surgery itself was much quicker than my previous operations; just open up the chest, pull out the catheter, and sew me back up. I came to while I was in the OR and they had the catheter in a ziplock bag for me. I don't recall asking for it (although I was planning on it). Either I did indeed ask for it while I was drugged up, or they know that some patients want it.I was given a prescription for vicadin, but I didn't fill it since the pain wasn't too bad. Tylenol was more than adequate for the first night, and by the next day, the pain was manageable without any drugs. Indeed, the worst part of the whole operation was probably pulling off the bandages and tape (and attached hair!) from my chest two days later!
I healed much more quickly from this operation than when it was put in. I was pretty much back to normal 2-3 days later.
- Wednesday, 4 February 2004 -- Radiation planning; tattoos; discuss CT results
-
I headed over to Dr. Nautiyal's office first thing in the morning for my radiation planning. The whole point of the planning is to produce a 3D model of my body so that the radiation can be delivered only to those areas where there was disease. Hopefully, this means that important vessels and organs will be spared the bulk of the radiation. A second objective of the planning session was to make sure that they can reproduce my exact position each time I come in for treatment. A deviation of even a few millimeters can mean the difference between irradiating the right and wrong areas. This procedure involved a CT technician (Amy), dosimetrist (Chris), and Dr. Nautiyal.
While checking in for my appointment, they told me that they weren't sure if Dr. Nautiyal would be "in network" for Cigna, but simply to let them know if that's the case and they will automatically adjust the bill so that I don't have to pay anything. I wish every office were as proactive and reasonable!
First, I lay down on top of a plastic bag filled with little beads. After the bag had molded around my upper body, they sucked all of the air out using a vacuum pump and then sealed the bag. The bag will be used throughout my treatment to ensure that I am always in the exact same position.The next step involved shooting alignment lasers onto my chest and using a marker to note several alignment points. Chris later used a syringe filled with ink to permanently tattoo seven of these alignment points onto my skin. The tattoos are not large (they are like tiny blackheads), but I am not very happy about having to get them. Aimee pointed out the irony of my having to receive tattoos, since I absolutely hate tattoos!
I ended up with three tattoos spaced across my chest (below my nipples), three more evenly spaced above my diaphragm, and one on the tip of my chin. The one of my chin is probably the most annoying since it is quite visible. Amy thinks that it will probably fade off eventually due to shaving. If not, there's always laser surgery to get rid of it!
After everybody was sure that my position could be reproduced, I was sent through the CT scanner one more time. I had to receive another injection of the IV contrast, but didn't have to drink the oral contrast. The scans will be fed into their modelling software, which will determine where and how much radiation will be delivered. These CT scans were much easier than the ones at Body Imaging because I didn't have to hold my breath.
Before leaving, Amy showed me my scans on the workstation. 96 scans were collected in all, each one representing a tiny sliver of my body. It is fascinating to see all of the different organs in the body, as well as foreign bodies (like dental fillings) that cause the x-rays to scatter and form artifacts on the display. They had also taped several metal ball bearings on my body to aid in the computer modeling, and these were quite visible on the scans. If you have any doubt at all about the importance of the CT scanner in modern medicine, and whether or not its inventor should have received the Nobel prize, read this article on the Naked Scientist.
Previously, I had asked Dr. Nautiyal if I was going to be fitted for "body armor" to protect the rest of my body from the radiation (just like in the dentist's office). He chuckled and said that the radiation that they use would cut right through anything like that. Their radiation "gun" (I'm not sure what it's called) generates 7 million volts and requires 10cm of lead for shielding! They will place these 10cm blocks on the gun itself since they would be far too heavy and bulky to be placed on me directly.
After we were all done at the radiation planning, we grabbed a bite to eat down the street and then went to Dr. Karamlou's office to discuss the results from my diagnostic full-body CT scan on Monday.
It felt strange (but good, obviously) not to be getting chemotherapy. I still went through the regular office ritual (weight, blood pressure, pulse, temperature, complete blood count), but luckily I didn't experience any anticipatory nausea. It looks like my body is smart enough to realize that it's all done with treatment.
Dr. Karamlou told me that the CT scan results were as expected. All of the tumors in my lower body have disappeared completely. Before starting treatment, it wasn't clear if the enlarged lymph nodes in my lower body were tumors or something else. Their disappearance in response to the chemotherapy proves that they were tumors and that I was definitely in stage III of the disease.
The largest tumor in my body (in my mediastinum) has shrunk to 2cm. While I had hoped to hear that it had disappeared completely, both Dr. Karamlou and Dr. Nautiyal say that this is expected behavior. The tumor will probably continue to shrink as the chemotherapy drugs finish up their work. And, of course, the whole area will be getting irradiated anyway. Lastly, when very large tumors shrink, they often leave behind permanent scar tissue. The scar tissue is benign, but the CT scan doesn't differentiate. The only way to know for sure is a PET scan or to monitor the area to make sure it doesn't grow.
Since Dr. Karamlou wasn't around last week during my final chemo, I tried to express my heartfelt gratitude at everything that he's done for me, but he adroitly resisted my efforts to get mushy. I was hoping to look him in the eye and convey a sincere "thank you" for everything that he's done for me. I think this is something that far too few patients tell their doctors nowadays. Considering all of the years of study, not to mention the continuing demands on their personal lives, I feel it's the least that we can do! Sure, that's why they make the big bucks, but you can tell that doctors like Dr. Karamlou don't go into it for the money.He is such an easy going doctor that our consultations seem more like hanging out with a friend than an office visit. I am so glad that he was the doctor that accompanied me through this experience. Looking back on all the advice I received early on, the people who said to choose the doctor that you're most comfortable with were spot on. As I look to the future, I realize that Dr. Karamlou and I are going to be together for many years to come (at least five years of follow-up visits, unless one of us moves away).
- Tuesday, 3 February 2004 -- Port removal (almost)
-
I went to Dr. Khaki's today. I thought I was going to have my port removed in his office, but he wants to do it in the OR. He said he can do a much better job of removing the port and closing up the wound (using cauterization instead of sutures), the lighting and equipment is better, it's more sterile in there, etc. I suppose it's also a good place to be if something goes wrong!
He'll be on vacation next week, so we scheduled the surgery for 23 February.
- Monday, 2 February 2004 -- Restaging CT scan
-
Happy birthday to me!
I went to Body Imaging for my restaging CT scan, covering my head, neck, chest, abdomen, and pelvis (pretty much my whole body except my legs). The procedure took quite a while because it was essentially three different scans. I had to drink a barium contrast solution about an hour before the scan, and also received two separate injections of IV contrast.
After the scans were done, they had me wait on the scanner for about 15 minutes while they made sure that all of the scans turned out ok. This gave me a lot of time to think about what the results will end up being and whether I am cured or not. The best birthday gift in the world would be a clean bill of health.
As part of the clinical trial, I will be getting CT scans every six months for the next three years, and then once a year for years four and five. I won't get any scheduled scans after that, unless there is some medical reason to do so. For future CT scans, I plan on wearing a "CT scan outfit" that has no metal whatsoever so that I can avoid having to change into a hospital gown.
The past few times I've been in for an x-ray or CT scan, I've asked the technician how much radiation these procedures generate. Their answers have been pretty unsatisfactory, so I hit the web: The FDA has a pretty good explanation of the radiation risks from CT (fda.gov):
A chest x-ray is equivalent to 2.4 days in the sun (0.002 cSv).
A head CT scan, 243 days (0.2 cSv).
An abdomen CT scan, 3.3 years (1 cSv).
My upcoming radiation treatment: 11,880 years (3600 cSv)!The FDA site also has a good explanation of the differences between the various measurement units used in radiation: rads, grays, sieverts, and rems. I calculated the 11,880 year figure above assuming that the weighting factor for radiation treatment is 1 Sv = 1 Gy. Next time I see Dr. Nautiyal, I'll see if this is correct or not.
I also had a chest x-ray done while I was there (for the clinical trial). While the full radiology report wasn't done by the time I left, I peeked inside the folder and saw a note that said "no active cardiopulmonary disease".
- Thursday, 29 January 2004 -- Radiation oncologist consultation; depressed
-
Aimee and I met with Dr. Nautiyal today to go over the next phase in my treatment, the radiation therapy. I was also supposed to receive a planning CT scan, but their CT scanner wasn't working. The planning CT scan helps them figure out where exactly (down to the millimeter, if I understand correctly) to shoot the radiation beams. This will be rescheduled for next week.
While we were waiting to see Dr. Nautiyal, my eyes came to rest on a door at the end of the hallway with the international radiation symbol on it. One of those "do-not-enter-while-light-is-on-because-you-will-get-fried" lights was also above the door, clicking on and off. Even though I have known what was coming for many months, the reality of the situation hadn't really sunk in until I saw that door.
Dr. Nautiyal started off by doing his signature super thorough physical examination. He then wanted to stick the fiberoptic tube scope in my nose and look around again. The two previous times I've had this done, I felt that the anesthetic (lidocaine) that they used was much worse than the procedure itself. So I went without it this time and tolerated the procedure much better.
We then discussed the possible long term side effects of the radiation. It's pretty much the same list as he discussed on our first visit back in November:
- 30% chance my thyroid gland will be destroyed. I already knew about this, although last time I was told it was 15 percent. My chances are getting worse! This can be rectified easily enough through daily medication if it happens.
- 10% chance of secondary cancer down the road (like leukemia). This would seriously suck. However, it would suck much worse to not completely cure my existing disease and have to go through a stem cell transplant.
- A chance that my parotid glands (saliva production) will be affected, resulting in dry mouth. I will definitely be receiving radiation on the left side of my neck; if I receive it on both sides, the chances of something going wrong in my parotids goes up.
- A small chance of getting L'Hermittes Sign, a condition where the hands and spine "buzz" (electric shock sensation) when you touch your chin to your chest.
- A very small chance of paralysis.
Pretty scary stuff. On the bright side, the treatment itself only takes a few minutes a day and is not painful at all. It is supposed to be like receiving a diagnostic x-ray. The only expected side effects during treatment are fatigue, sore throat, and dry/sunburned skin.
One thing that caught me off guard was the size of the area that will be treated. I had thought that it would just be my mediastinum, but it turns out that the 7.5cm tumor that was originally present there extended up the left side of my neck. The trial requires a buffer zone of 5cm above and below where the tumor used to be, so my total area to be treated will extend from just below my jaw all the way down to my diaphragm. Dr. Nautiyal seemed surprised that we were surprised. He is very thorough; I'm sure he probably mentioned this back in November when we talked to him, but with everything else going on, it may not have sunk in.
Hearing that I'm going to have such a large area zapped freaked me out quite a bit. I figured that the heart, lungs, and other important body parts in the treatment area would be at risk for damage, but Dr. Nautiyal doesn't seem to think that there is much risk at all. Decades of radiotherapy research and treatment have determined the tolerance of various organs, and my treatment dose (3600 cGy) is well below the problem threshold for most of the organs (7000 cGy for the heart, for instance).
The same old question that comes back to haunt me again and again is whether one month of radiation is less toxic than three more months of chemotherapy would have been. There has been a significant amount of evidence showing that patients with bulky disease tend to relapse in the bulky area if they relapse at all. So there's a lot of motivation behind giving extra treatment to bulky areas of disease. On the other hand, because Hodgkin's Disease strikes so many young patients, there is a strong desire to treat as little as necessary in order to avoid secondary cancers down the road. Read this Medscape article (free registration required, scroll to the paragraph starting "The third plenary") or this excellent Blood journal paper (search for the paragraph starting "A recently published") for more information.
As far as I can tell, whether to radiate or not after chemotherapy is the biggest debate right now in treating Hodgkin's patients. Of course, the most important thing is to cure the disease that is currently present rather than try to prevent a future disease that may not even happen and, in the process, undertreat the current disease. I have heard that your best chance at being fully cured comes with your first attempt; relapses are really bad news since the body is much weaker and the cancer comes back tougher.
So, charge up the ray guns, I'm going forward with the radiation therapy. I'm definitely feeling very depressed today, the most depressed I've been since way back in October when I was initially diagnosed. Sitting down with Dr. Nautiyal and going over the gloom and doom list of all the things that can possibly go wrong was a little too much for me to handle. I suppose in a way it makes sense since it feels like I am starting treatment all over again, and thus will be going through all of the psychological stages that I went through before starting chemotherapy. Hopefully I will feel better once I begin treatment.
- Tuesday, 27 January 2004 -- Chemotherapy #12 (last one!)
-
Last chemotherapy!
I didn't meet with Dr. Karamlou, so it was a quick visit. I only had to receive one quick drip bag (Bleomycin) and one injection (Vincristine) and I was out of there. A little underwhelming and anti-climatic, but that actually corresponds to how I feel. I have been in the chemotherapy routine for so long that it feels weird to be done. The last time I felt this way was after final exams in college: Downshifting my brain instantly from full-speed to zero left me with a full tank of gas and nowhere to go. Also, I am not really done with treatment, as I still have the radiation to go. Depending on how you measure it, I am either 50% done (objective-based) or 75% done (time-based).
Nevertheless, it feels really, really, really good to be done with chemotherapy. Looking back, it wasn't as horrible as I was expecting, but it's definitely something I never want to go through again.
I thoroughly enjoyed throwing away my sharps container, another symbolic victory since I should never need Neupogen shots ever again. My port, which has been growing sorer each week, seemed to hurt more than ever this time. It felt good to know that it will be taken out next week, never to be accessed again.I felt a pang of sadness since my time with everybody at the office is drawing to a close. I have shared an intense, life-saving experience with these people, and I will never forget any of them... especially Nancy and Carol (and, of course, Dr. Karamlou, but I'll cover him in next week's journal). Without their help and support, this entire experience would have been much more difficult. I am overcome with gratitude that they have chosen to dedicate their lives to helping patients overcome cancer. Oncology can't be an easy field of medicine, with all the suffering and patients dying off all the time.
Near the end of my treatment, Carol and Julie showed up with a surprise: A congratulatory card, flowers, balloon, and coffee mug full of chocolates. It was a very touching moment, and combined with the sentiments I just mentioned, my eyes started to get a little juicy.
I exchanged a round of hugs with everybody and then headed home to sleep off the effects from my last round of chemo! (It feels good to stick "...from my last round of chemo" on the end of everything!)
- Monday, 26 January 2004 -- Medication reduction; bills update
-
Today is the last day for my many of my medications, including:
- Last neupogen shot!
- Last Prednisone!
- Last Nexium!
This is very exciting for me as remembering to take my medications, and remembering which medications to take on which days, has been somewhat stressful for me. I'm looking forward to not having to worry about if I forgot to take my pills, not getting poked in the arm every day, and not having so many drugs swirling around in my body.
I have been using two pillminders and a medication log to keep track of it all. (If you need a TIFF viewer for the medication log, I recommend AlternaTIFF.)
I spoke with Dr. Nautiyal's billing office today and they have agreed to waive the part of my bill that is above the reasonable and customary amount that Lumenos has already paid. Dr. Khaki's office and Oregon Hematology appear to have done the same, as they haven't tried to collect any balance due from me either.
Speaking of insurance, I found a lost journal entry that I had forgotten to post from way back in December. You can read it here.
- Thursday, 22 January 2004 -- Terrible sleep; constipated again
-
I had a terrible night's sleep last night and felt lousy all day. I'm not sure if I feel bad because of the lack of sleep, the lack of Prednisone, or from the recent chemotherapy treatment. I'm also constipated again.
- Wednesday, 21 January 2004 -- Chemotherapy #11b; dehydrated
-
The Emend has been doing its job and I have not been too terribly nauseated, but drinking is a huge problem. Given my recent constipation problems, I am especially cognizant of the need to stay hydrated. Water and other drinks are just not appealing for whatever reason.
I mentioned this to Nancy, who gave me a couple extra bags of saline via IV to help hydrate me. All in all, I ended up with 1 bag of Etoposide and 3 bags of saline, for a total of between 1.5L and 2.0L of liquid. "Drinking" in this manner is definitely convenient! If only I could figure out some way to do it while doing mountaineering and other intense sports... maybe a new product line idea for Camelbak.

Asleep again
Drip bags
Taking a callThis video shows the view most of the time while receiving chemotherapy. (If you are having trouble viewing the video, try Quicktime.)
- Tuesday, 20 January 2004 -- Chemotherapy #11a; anemic
-
Today was my last "bad week" treatment ever! Even though I knew in my mind that it wouldn't be as bad as the treatment was two weeks ago, I still psyched myself out ahead of time and ended up really nervous and nauseated.
When I met with Dr. Karamlou for my pre-treatment consultation, we discussed my constipation from the previous weekend. I also mentioned my recent leg weakness and how my portacath has been hurting me all week. Every so often, I start to worry that my portacath has formed a blood clot and is about to kill me (this is usually precipitated my some miscellaneous body ache in my chest). But in this case there was obvious bruising all around the port, so I probably just whacked myself during the week without realizing it.
As for the leg weakness, I had blamed it on vinblastine, but Dr. Karamlou thinks it was a result of having been on such massive doses of Prednisone for an extended period of time. He told me that most other regimens that use large amounts of Prednisone (treating non-Hodgkin's lymphomas, for instance) only go for 5 days or so and then take a break. I have been on 70mg every other day for over two months! Needless to say, I am thankful that I am tapering down and will be completely off of it by the end of the week. I still don't know exactly what it is that the Prednisone is doing or how it fights cancer, but I have talked to enough people to know that it is a very powerful corticosteroid that shouldn't be messed with lightly. I am happy to be done with it.
[Update, 5 February: According to Chemocare's Prednisone fact sheet, the main side effects are increased appetite, irritability, insomnia, heartburn, muscle weakness, headaches, dizziness, mood swings, eye problems, increased sun sensitivty, and weakened immune system. These are only the side effects that I've experienced; see the article for the full list. The site also has a good description of how Prednisone fights cancer: It decreases swelling around tumors and alters the body's normal immune system. Prednisone can even be used by itself without chemotherapy to treat some very early stage cases of lymphoma.]
After so many weeks of being in the same old chemotherapy routine, it was exciting to discuss the next steps I'll be taking from here:
- After my last treatment, I will be restaged to determine how much (if any) disease is left in my body. This will involve a full-body CT scan.
- I'll have my evaluation meeting with Dr. Nautiyal in which they will do all the 3D modeling and simulations necessary for the radiation treatment. This will also involve several CT scans. I've stocked up two bottles of the yummy barium contrast in my fridge in preparation for all of this scanning.
- I can have my portacath removed any time after the last treatment! Having the portacath removed is a huge psychological milestone, not only because it means never having to get another chemo treatment, but also because of all the pain and nausea that I have associated with it. I had read on the Internet that many patients leave their ports in for many months after treatment in case of relapse, but Dr. Karamlou didn't seem concerned about that at all.
My bloodwork this week showed that I have officially crossed the line into being anemic. Normally this would mean that I would start taking Procrit shots (red blood cell booster) in addition to the Neupogen shots I am already taking. But since next week's treatment is the last one, and it's not immunosuppressive, Dr. Karamlou advised not getting the shots. My body will start getting better on its own once chemo ends.
The actual treatment itself was uneventful as usual. I was cold again and had to pile on two blankets to get warm. I tried to watch a DVD, but ended up falling asleep almost immediately. I remember the early days of chemo when I was full of energy and would see other patients dozing away in their chairs. Now I have become those other patients.
Aimee and my mom kept me company throughout the entire treatment.
- Monday, 19 January 2004 -- Medical leave of absence; last day of work
-
I have finally thrown in the towel and decided to go on short term disability from work. I was barely holding on before the end of the year, and now the slow gradual decline of chemotherapy has taken its toll.
It's a combination of things: I get extremely tired in the afternoons and have to take a nap. I have trouble concentrating for more than a few minutes on complex tasks. I have horrible sleep patterns that make it hard to get up and to work at a reasonable time. And, of course, there's the actual chemotherapy treatments themselves and their side effects. Plus, at best, I have been working at 25% efficiency, which isn't fair to the people I work with.
Everybody at work, from my colleagues all the way up the management chain, has been so wonderfully supportive. It makes me feel very grateful to work with such good people at a good company. I remember not too many years ago when the siren call of the Internet bubble was luring everybody away to startups. Startups with no benefits, but plenty of stock options, so nobody cared about the benefits. I thank my lucky stars that I didn't end up working for one of those companies... After I get better, I look forward to staying right where I am for many happy years of work.
Anyway, for now, I am looking forward to focusing 100% on getting better and not having to worry myself with the quotidian concerns of the working world.
Because I signed up for Short Term Disability insurance last year, I'll get about $500 a week for the first 12 weeks of disability. My company is generously making up the difference (they call it "Salary Compensation") between my regular salary and what the insurance pays. After 12 weeks, the salary compensation goes away and the disability insurance pays more, but I plan to be back at work by then anyway.
- Sunday, 18 January 2004 -- Dance Dance Revolution; tubby
-
I had dinner with Ben, Annie, and the rest of the gang at the Big House tonight and tried to play Dance Dance Revolution afterwards. I realize now just how much of a tubby I've become. I started out well enough, but hit "the wall" after about a minute of dancing. It felt as if I had been exercising all out for a much longer period of time, like trying to sprint a mile at full speed. My heart was pounding intensely and I felt as if I might throw up. My whole body went clammy and I broke out in a cold sweat. I was able to walk around again after a few minutes of sitting down, but it took over an hour for my body to fully return back to normal!
I am limiting myself to walking for exercise (and maybe slow Dance Dance Revolution songs) from now on :-)
Speaking of getting fat and lazy, I am acquiring quite a pooch and many of my pants are tight around the waist now. My body fat is hovering around 10 percent now, almost three times the level after I finished my bike ride across America (3.5%).
- Saturday, 17 January 2004 -- Blood in stool
-
I am starting to feel a lot better, although I am still tired all the time. I am looking forward to my blood count test next week to confirm my suspicions that my red blood counts are still dropping.
I hadn't had a bowel movement since Thursday, but was finally able to squeeze something out by exerting myself quite a bit. I was shocked to see a tablespoon or so of bright red blood in the toilet bowl afterwards. "Blood in stool" is on the "call immediately if this happens" list, so I called the office, even though I always feel guilty about bugging folks on the weekend.
As it turns out, Dr. Karamlou was the doctor on call. He told me that I had probably torn something by exerting myself too hard and also that I am really constipated. Whatever the cause, it certainly hurt quite a bit, sort of like straining yourself while doing weight lifting squats. He advised heavy doses of fiber, laxatives, and stool softeners to get things flowing normally again.
Ever since I started chemotherapy, I have been warned that constipation would be a problem. I have been lucky up until now, but, like so many other things, the cumulative effect of the chemotherapy has finally caught up to me.
On an interesting note, I learned later that Dr. Karamlou is on call every fifth weekend or so. And that some of the other doctors at the office pay retired oncologists to cover for them when it's their turn to be on call. Aaah, the behind-the-scenes mechanics of running a medical practice... very interesting!
- Thursday, 15 January 2004 -- Chest x-ray results; radiation doubts; knee weakness
-
[Editorial note: Folks have been asking about how I post updates, especially
when they see a new update, but the date on it is quite old. Basically, with my
feeling so tired lately, I have not felt like typing away on the computer. I
usually jot down events as they happen on a notepad, and then go back when I
feel like it and retroactively write the journal entry.]
I forgot to mention two important things from yesterday's office visit.
First, Dr. Karamlou told me that the radiology results from my most recent chest x-ray were completely normal -- no mediastinal mass reported whatsoever! Because the x-ray was done at St. Vincent's, the radiologist didn't know about my prior x-rays/history from Good Sam, so the analysis is coming from a fresh perspective.
This is obviously great news, but it has raised the whole Stanford-V-versus-ABVD debate in my head once again. My body is obviously responding very well to chemotherapy; would I have been better off doing 3 more months of chemo (ABVD) instead of the 1 month of radiation that is to come with Stanford V? I suppose I will wonder about this for the rest of my life or until some clinical trial proves which treatment is superior.
One option would be to just skip the radiation and call it done (I'm sure Carol or Dr. Karamlou are freaking out right now if they are reading this), but I realize that my best chance to full recovery is not to e2e with the proven treatment regimen, designed by Hodgkin's experts at Stanford with the express purpose of being more effective and less toxic than existing treatments. At least that's what I keep repeating to myself when doubt lingers in my head in the small of the night.
Second, during my physical exam yesterday, Dr. Karamlou tried to do the classic doctor's-tap-on-the-knee-to-make-the-leg-move-by-itself maneuver, and it wouldn't work! Some people simply don't have reflexes, but I know that this usually works on me. Yet more nerve damage from the vinblastine I fear. My legs have been extremely wobbly of late, particularly while traversing stairs. In addition, my knees often feel weak, like they could give out at any moment. Sure enough, I dug out the trial consent form, and under the listed side effects for vinblastine are "unsteadiness when walking (may last for months)" and "loss of reflexes (may last for months)". I vaguely recall being worried in an academic sense when I read these warnings before treatment, but it definitely becomes much more worrisome when it happens for real! At least they use the term "may last for months" instead of "may be permanent".
- Wednesday, 14 January 2004 -- Chemotherapy #10, anticipatory nausea, Prednisone taper
-
The chemos are starting to catch up to me. This was supposed to be an "easy" week, but I felt almost as bad as during the hard weeks.
For the past few office visits, I have been getting nauseated even before treatment starts. I start feeling bad a few hours before my appointment time and then progress to really bad while waiting to talk to the doctor. I mentioned this today and was told that I have "anticipatory nausea", common among chemotherapy patients. As it turns out, the original purpose of the drug Ativan was to prevent pre-treatment nausea. I'm going to start taking it in the mornings before treatment from now on.
Other than that, it was good to be back at my regular office and to see everybody again. Dr. Karamlou was looking spiffy in a new shirt and tie. Apparently, he wasn't the only one who looked different, as Nancy commented that my face looked a little chubby. This is a known side effect of Prednisone called "Moon Face". I really hadn't noticed, but somebody at work mentioned it at as well.
The numbness in my fingers is getting worse, extending about the first inch of all my fingers on both hands now. I am not looking forward to this week's dose of vinblastine, which is going to make it even worse. My feet are becoming afflicted as well and often feel like they are "vibrating". My toes have been cramping too. Dr. Karamlou thinks I have a calcium deficiency and said that eating some Tums may help. I am going to try some glutamine and vitamin B6 for the finger numbness, although I am always reluctant to take too many extraneous supplements or drugs, fearing that they may interfere with the chemotherapy regimen.
Far and away, my biggest symptom lately has been fatigue. I am tired all the time. Dr. Karamlou said that this is an effect of long-term chemotherapy and that there is nothing that can be done for it. If I were anemic, then they could do something, but my bloodwork shows that I am fine.
Dr. Karamlou told me to start tapering my Prednisone dosage this week, taking 10mg less each time until I'm not taking any at all. (I have been taking 70mg every other day for the last 9 weeks.) This is a big milestone as it is yet another indication that the end of chemotherapy is drawing near! I also hope to rid myself of some of the more unpleasant side effects of Prednisone, namely the paranoia, anxiousness, and insomnia that have plagued me for the past two months.
- Monday, 12 January 2004 -- Cytoxan and ear ringing
-
According to Chemocare.com, Cytoxan (Cyclophosphamide) is a Nitrogen Mustard derivative. And one of the side effects of Nitrogen Mustard is ringing in the ears. Ergo, I think the ringing I've had in my ears for the last six weeks must be related to Cytoxan and not to some mysterious ENT problem. That's a relief, as I presume the ringing will go away once chemotherapy ends.
By the way, here is a great explanation of the different types of chemotherapy drugs. It explains alkylating agents, plant alkaloids, antitumor antibiotics, and topoisomerase inhibitors (all of which are part of my treatment) and the role each plays in fighting cancer.
- Friday, 9 January 2004 -- Headache; very tired; Dr. Khaki
-
I had a great night's sleep and woke up with only mild-to-moderate nausea, but I had a pounding headache from the anti-nausea drugs (either the Kytril or the Emend or both). Ahh, the dilemma: Headache or nausea? Actually, the choice is pretty easy, I would choose the headache every time. Nausea is just too debilitating. I was able to manage the headache well enough with a bunch of Tylenol and Advil, although I had to max out the recommended daily allowance. Most importantly, I was able to eat and drink somewhat normally.
I am feeling incredibly tired all the time. I think the chemo is starting to take its toll on my red blood cell levels. I can't go more than a few hours without needing to take a nap on the couch. When I'm awake, I find that I can't stand up for very long. I like to just sit and listen, like an old grandparent or little newborn who sits in the corner while the rest of the family leads their energetic lives. For me, this feeling of lethargy is perhaps one of the worst symptoms of all as it makes me feel absolutely feeble and helpless. I also feel hot a lot of the time, especially my upper body and face; I'm not sure if that's related.
Dr. Khaki surprised me with a call today. He was just touching base to see how my treatment was going and to make sure I wasn't having any problems with the portacath. I was really impressed and touched that he took the time to call personally and check in on me.
- Thursday, 8 January 2004 -- Chemotherapy #9
-
Dr. Karamlou was at the Gresham office today, but the roads were so treacherous with ice that they decided to route the patients to the other offices. Around lunch time, they called and asked if I could be at the St. Vincent's office "as soon as possible". Normally the trip takes about 15 minutes, but it took us over an hour to get there today as we had to shovel the car out of the snow, put on and take off chains, drive much slower than normal on the roads, etc.The office wasn't as packed as I was expecting; I think many of the patients were deferred until next week. I was glad to see that Lynn was going to be my nurse again. She remembered all of my "chemo preferences" from last week which was nice. She surprised me by telling me that she had checked out my web site... man, word spreads quickly about this site!
I felt like much more of a regular than on my first visit and was a lot more comfortable. The big open room atmosphere of St. Vincent's is starting to grow on me. I didn't really get into any conversations with people, but I did exchange friendly glances with the other patients, most of whom were elderly. They don't have DVDs available for check out here, but I listened to my iPod for a bit and read some magazines. Every now and then, my curiosity would be piqued by an overheard conversation fragment (usually medical jargon, such as one of the nurses telling the patient what he is getting) and I would listen in on that for a while to see if I could learn anything.
There was one super sick looking guy, about 25 years old. He looked like a classic chemo patient, very pale and no head hair whatsoever. He seemed like he was in a lot of pain and just lay there with his eyes closed. I overheard the nurse giving him instructions on his medication and heard several references to morphine, red blood cell boosters, white blood cell boosters... the gamut! I really can't complain about my treatment when I see guys like that.
My actual chemotherapy was pretty straightforward, except for obtaining Emend, the anti-nausea medicine that I take on hard weeks. At Good Sam, they give me free samples, but apparently St. Vincent's has been cut off by Merck for giving out too many. Lynn tried to call in a prescription for me, but both the hospital pharmacy and my usual pharmacy at Safeway don't stock it! As it turns out, they did have some samples over at Good Sam, so Aimee braved the treacherous streets to go and get it for me. While she was picking it up, she saw other patients getting treatment there... it turns out I could have gone there to begin with! A little miscommunication, not that big a deal. I would have driven up to Seattle if necessary for treatment!
I wrapped up the visit with a quick trip to the hospital radiology department for a chest x-ray (documenting my progress after month two for the clinical trial) and then headed home to sleep off the chemo.
- Wednesday, 7 January 2004 -- Chemotherapy postponed again
-
The city is still snowed and iced in, all the Oregon Hematology offices are closed, and my chemotherapy is now scheduled for tomorrow at the Gresham office. These delays are really stressing me out. I just really, really, really hope that it happens tomorrow.
- Tuesday, 6 January 2004 -- Awesome sleep; delayed treatment
-
I had the best night's sleep since I began treatment last night: I took a one-hour nap before bed time from 9-10pm, watched a little TV, and then went to sleep around midnight. No need for Ativan or Ambien. I fell asleep effortlessly and woke up eight hours later at 8am. There's nothing quite like the simple pleasure of a good night's sleep.
The bad news today is that my chemo treatment was postponed until tomorrow. Dr. Karamlou and some of the office workers were unable to get to work because of the snow and ice in Portland. The other offices around Portland (St. Vincent's, Gresham, Tigard) were already closed or closing early as well.
Delaying treatment makes me really nervous. It probably doesn't make a difference if the delay is only a day, but I like to stay exactly on the protocol schedule to maximize my chances of full recovery. I shouldn't complain too much: Without the Neupogen shots, my treatment would have been delayed several times already due to low white blood cell counts.
Still, delaying this week's chemo kind of stinks since I know it is going to be a really nasty treatment. I want to get it over with! I just hope that the offices are open tomorrow! Delaying two days would really stink.
- Monday, 5 January 2004 -- Dr. Dierks
-
I finally saw Dr. Dierks today after almost two months of waiting (three weeks of waiting due to his busy schedule and another month of waiting because he wouldn't accept my old insurance). I was hoping to get three issues resolved from my visit:
First, Dr. Nautiyal wanted Dr. Dierks to give a second opinion on some tissue in my nasal pharynx and whether it's cancerous or not. He jammed a fiber optic in my nose, had a look around, and said that nothing jumped out at him. He wants me to get a CT scan of my head just to make sure (my previous two CT scans only covered my neck, chest, abdomen, and pelvis).
Second, Dr. Karamlou wanted Dr. Dierks to examine the fluid build up in my ears. Dr. Dierks surprised me by saying that he is a cancer/surgery ENT and and that I need to see a general ENT! He looked in my ear anyway and said that it looked normal to him, which also came as a complete surprise. Dr. Karamlou has been reporting fluid in it for months. The ear still hurts, so something has to be wrong in there. I'll ask Dr. Karamlou about it again tomorrow.
Finally, I wanted Dr. Dierks to solve the throat clearing problem that I have had for over three years (which my friend Suzanne thinks is a mild form of Tourette Syndrome). He said that it might be caused by acid reflux bubbling up from my stomach into my esophagus. Apparently both he and his office partner also are afflicted with the same problem. He suggested cutting back on caffeine and trying Tums.
All in all, the visit was not the epiphany I was hoping for, but I guess no news is good news!
- Friday, 2 January 2004 -- 150 pounds!
-
After months of forcing food into my mouth at every available opportunity, I finally reached my target weight of 150 pounds (150.2 to be exact)! Sadly this means that I need to curtail my diet of Jimmy Dean breakfast sausages and other high fat foods and start eating more healthily. It's probably a good thing since I am starting to form a bit of a pooch.
- Thursday, 1 January 2004 -- New insurance at last!
-
I'm officially back on Cigna for insurance as of today. Hopefully this will mean less hassle and lower out-of-pocket expenses.
I had the worst night's sleep since I began treatment last night, only about two hours total. Lying in bed with nothing to do is unbearable, so when I can't sleep, I just park myself in the living room and watch TV or play XBOX until I just fall asleep on the couch.
XBOX, by the way, is essential for surviving chemotherapy. Everybody knows that watching TV is a pretty mindless activity. There is only so much you can take before going insane. XBOX games, on the other hand, constantly stimulate your brain and keep you occupied for hours on end. I've been playing a lot of Grand Theft Auto: Vice City, Dungeons & Dragons Heroes, and Simpsons Hit & Run.
When the light woke me up in the morning, the city was covered in 5-6 inches of joyful fluffy powdery snow! I haven't seen accumulation like this in a long time. Aimee and I went for a long walk to downtown through the snow. There were very few people out and about, so it felt like we had a winter wonderland to ourselves. We saw several groups of people cross country skiing through the city and others building snowmen all over the place. What a different city Portland would be if it snowed instead of rained all winter long!After the walk, I was feeling pretty sick/tired, and I spent the rest of the day sleeping on the couch.
Here's a panoramic view of the snow from my condo deck:
- Wednesday, 31 December 2003 -- End of the year
-
The end of the year is here at last. The time has really flown by. I still can't believe I'm 70% done with chemotherapy. Paradoxically, I can't believe that it was just back in October that I was diagnosed and all of this started. It still seems like yesterday.
I decided to completely forego all of the New Year's Eve parties that I was invited to, even the one conveniently located across the street. I am too tired to stand on my feet the whole night, yet I would feel like a loser if I went to a party and just sat on the couch the whole time. Similarly, the extrovert in me always likes to meet new people at parties, yet I don't have the energy or motivation right now for that.
And, based on my experience with other holiday parties earlier in the month, I know that anybody who knows me would either ask for for an update or need to be told, neither of which I really felt up to. Basically, I'm taking myself out of the party social scene until I recover. I still look forward to visitors at the condo, though, for anybody out there who has been thinking about a visit :-)
Instead, Aimee and I enjoyed a quiet evening at home playing XBOX and watching Tivo. We went out on the deck at midnight, listened to the cheering crowds from Pioneer Square, and watched the fireworks displays from downtown, from across the river in Vancouver, and, from dozens of people launching their own fireworks along the Columbia River Gorge. We were both amazed that we could see the fireworks since the Gorge is so far away.
- Tuesday, 30 December 2003 -- Chemotherapy #8; St. Vincent's office; 2/3 done!
-
Today was the end of my second cycle of chemo. I'm now officially two-thirds done! Only one month to go. The end is so close, I can taste it: One more "really bad" treatment (week 9), one more "medium bad" treatment (week 11), and then the other two weeks should be a cake walk.
I had to go up to the main Oregon Hematology office at St. Vincent's hospital for this week's treatment. I call it the mothership, since it's the original, biggest, and busiest location. Dr. Karamlou was sick and unable to come into my regular office (Good Samaritan hospital), so all his patients had to be rescheduled for other offices. For legal and medical reasons, a doctor has to be on premise if patients are being treated. Ironically, I didn't see a single doctor during my visit to mothership; the nurses take care of everything by themselves.
Dr. Karamlou's illness coincided with another major incident, the great end-of-year snow and ice storm in Portland! When it snows in Portland it pretty much shuts things down completely, so I was really nervous about making sure I got in for treatment. Normally, being snowed in is fun, a chance to take the day off from work and mess around. When you have a critical appointment like chemotherapy, though, it can be unsettling. Aimee and I knew that it might be impossible to drive a car down the super steep hill from my condo, so we left her car on the street at the bottom of the hill. We also could have taken the train out to St. Vincent's in a worst-case scenario. I just crossed my fingers that the office staff and doctors would be able to make it as well! Through rain, snow, sleet, and hail, the chemo must go on!
My weekly office visit ritual has grown into a bit of an intimate bond with the people involved and it felt weird to be doing it with strangers. We were all on autopilot and things went fine, but it makes me really appreciate my regular crew: Teia, Julia, Nancy, Julie, Carol, and Dr. Karamlou.
I am sure it is a matter of being used to your favorite office, but I am glad I'm not getting my treatment at the mothership. The chemo area has three times as many chairs as Good Sam, and things are pretty cramped. And crowded. And hectic. Almost all of the chairs were occupied while I was there. There is a lot less privacy and you are pretty much in other patient's business. And there didn't appear to be any DVD player checkouts available either :-(
The crowded quarters aside, the staff were very friendly, efficient, and competent, as I have come to expect from Oregon Hematology employees. My nurse, Lynn, was very nice and attended to my little idiosyncrasies with aplomb (blast of numbing spray before getting ported, letting me double check the dosage of each chemo bag before it is hooked up to my IV, giving me a copy of my blood counts for my records, etc.).
One beneficial side affect of the close quarters is that the patients were pretty talkative with each other, something that never really happens at my regular office. It was lot like happy hour at Cheers, with people sitting around, nodding their heads in agreement while somebody spoke of some medical procedure, or chiming in with their own additions. There were quite a few people sleeping (and snoring :-) and a few pissed off looking people, but all in all, it was nice to see the shared camaraderie.
By the way, I absolutely love week 4 of the cycle. Two small drip bags, one tiny push injection, and you're outta there! Plus, as a bonus, no real nausea to speak of.
- Wednesday, 24 December 2003 - Chemotherapy #7b
-
I donned a Santa hat for part two of chemotherapy this week to celebrate the holiday spirit. Ironically, people thought I was wearing the hat to cover up for missing hair :-)
I was expecting the chemo ward to be deserted like yesterday, especially since it was Christmas Eve, but it was totally packed! Everybody seemed to have a visitor with them which made me feel good; I always hate it when I see people doing chemotherapy alone.
I talked with Julia quite a bit about the different types of blood cells, and she gave me a pretty cool book on the subject which I read to pass the time. The material was way over my head, but I enjoyed looking at the pictures. She even set up a microscope with one of my blood samples so that I could see this stuff "for real". For some reason, I never really got into the life sciences before (preferring physical sciences like engineering in high school and college), but now I can't get enough of them! I would love to have my own lab of state-of-the-art biotech equipment at home that I could use to explore the hidden wonders of my body...The Emend appears to be working. I felt a little bit nauseated after treatment, but not nearly as bad as on previous odd weeks. More importantly, I didn't lose my appetite or thirst. A couple of weeks ago, I lost almost five pounds after treatment and was really worried about dehydration. No problems with that this week.
- Tuesday, 23 December 2003 - Chemotherapy #7a
-
My parents are in town visiting for the holidays, so they came with me to
chemotherapy this week. I am glad that they got a chance to meet all of the
people who are helping me get better. This is the first time that Aimee has
missed a visit, and everybody in the office kept asking where she was. She
probably could have come, but I didn't want to have too many visitors in the
chemo area that might potentially bother other patients.
We met with Dr. David Something again this week and reviewed my progress over the previous week (typical even week symptoms: moderate insomnia, tingly fingers, dull bone pain). I learned that he is not in his fellowship as I had previously thought, but rather his residency and thus has quite a ways to go before becoming a practicing oncologist (15 years total education after high school graduation). He told us it was his last day in the office, so I wished him good luck with his medical career.
Dr. Karamlou came in next and chatted with us for a while. It was a pretty short talk since I really didn't have any complaints. My parents were really impressed with him and the rest of the people at Oregon Hematology, commenting that I am receiving excellent medical care after we got home.
In preparation for this week's treatment, Dr. Karamlou prescribed a new anti-nausea medication called Emend, from Merck. It is supposed to be really good for easing delayed onset nausea like I have been experiencing. The pill comes in a three-pack; you take one pill an hour before chemotherapy, and then one pill a day for the next two days.
We had the entire chemo ward to ourselves for treatment. My mom and I watched "Two Weeks Notice" on DVD while my dad read a book. For the first time ever, I started to get cold during treatment. Julia (one of the medical techs) noticed and gave me a nice blanket and a cup of hot chocolate to warm me up.I have formed a "hit list" of most hated chemotherapy drugs:
- Cytoxan, Adriamycin: The worst. I always feel terrible afterwards.
- Etopocide: Medium bad. I can feel the drugs swimming around inside me afterwards, and it doesn't feel good.
- Vinblastine, Vincristine, Bleomycin: Not too bad.
After treatment, I could feel "the orb" in my head, but otherwise felt pretty decent. I even felt well enough to have my mom give me a haircut since my hair refuses to fall out :-)
- Sunday, 21 December 2003 -- After the sixth week; hair is starting to fall
-
This week has been much, much better than last week. I have had little to no nausea and only my usual maladies apply: Insomnia, tingly fingers (it's spread to all fingers now), and ear ache. My upper legs ache a little bit too.
I having a difficult time staying hydrated. I am cognizant of the tremendous stress all of the drugs are putting on my body and try to give my kidneys and other organs as much liquid as possible. Lately, many of my favorite drinks (including, sadly, my one true love, Pepsi) have become unappetizing, and water tastes either bland or metallic. This has made drinking somewhat of a chore. I used to pride myself on being able to "pee clear" by the end of each day, but now my urine has some tint of yellow no matter how hard I try.
I have started a new system to help me drink more: Each morning I fill up three 1L Nalgene water bottles. I then drink from these throughout the day, pouring out an equivalent amount of water if I drink juice or some other drink. It helps tremendously to have a way to measure how much I've drunk and how much I have to go. As countless management books quip, you can't manage what you don't measure!
Lastly, my hair has finally started to fall out in significant quantities. Since the beginning, I have been bracing myself for the day when clumps of hair would detach spontaneously in the shower. That hasn't happened, and I don't think it's going to. Instead, I probably lose around 1,000 hairs a day. If this sounds like a lot, the average blond head has 140,000 hairs. I am definitely thinning, but I don't think it's that noticeable. See my daily pictures and decide for yourself.
A bunch of hairs come off in my hands while I'm shampooing; a whole lot more come off in the sink when I'm combing through my hair with my fingers. Then, throughout the day, I continuously shed hairs here and there. My clothes and other possessions (laptop, books, couch, etc.) are covered in short, light-colored hairs. Not all that different from any cat owner :-)
- Friday, 19 December 2003 -- Relieved; Neupogen shots; medical billing summary
-
I received my latest batch of "bills" (technically, they are called "explanation of benefit" statements) from Lumenos. They ended up paying Dr. Khaki's entire bill, no additional amount required from me. They still nickel and dime me 5 bucks here or there for each chemo treatment, but I am very much relieved that I shouldn't be forking over any more large out-of-pocket expenses this year.
I also learned that my earlier estimate for the cost of the Neupogen shots was way off... they are $415 each! It's hard to believe that every other week, I have over $2000 of injectible medications sitting in my refrigerator. This was an unexpected $10,000 total expense that will cause me to have way underestimated in my guess for total treatment cost.
I am still constantly amazed at how the insurance bills trickle in for certain procedures. For example, a doctor's visit with an x-ray might generate three or four separate bills: The office visit; the x-ray procedure itself; and one or more radiology bills to analzye the x-ray. The bone marrow biopsy is another example of a procedure that generated four or five separate bills.
Based on my recent experiences, I have formed this overview of how medical billing works:
- You go and see the doctor.
- The doctor does what he needs to do, blissfully detatched from all billing aspects of his practice. This is a good thing given how messed up it all is. It is better that he focuses solely on healing without regard to cost.
- The doctor's office bills your insurance some ridiculously high amount of money for your visit.
- If the doctor is in-network, the insurance company pays a significantly reduced amount, sometimes as little as 30-50% of than the original billed amount. The rest of the bill is written off. You're done.
- If the doctor is out-of-network, the insurance company will pay up to a certain maximum "reasonable and customary" amount. I don't really blame them for not paying the entire amount; they have to draw the line somewhere. Nevertheless, if your insurance is good, they will pay 90-95% of the bill.
- The doctor's billing office will then bill you for the difference, even though they are already making significantly more money than they would from an in-network patient.
- If you call and complain, they will probably write off the unpaid balance. I haven't had to resort to this yet, but if I ever get any problems, I will try to guilt them into writing it off by mentioning that the insurance company considers their charge to be beyond reasonable and customary and mention that they are already receiving more money than they would have from an in-network claim.
I guess I really can't blame either the doctor's offices or the insurance companies for how things have turned out. Given the large number of uninsured patients, the rising costs of providing best-of-class medical care to everybody, and countless other factors that I probably don't even know about, the system has evolved to its current state just to survive.
- Wednesday, 17 December 2003 -- X-ray results; chemotherapy is working!
-
Carol called me today to share the radiology results from my chest x-rays. I don't remember the exact wording from the report, but it was something along the lines of "significant reduction in mediastinal mass". The chemotherapy is working!
This is the first concrete evidence I've gotten regarding my body's response to the chemotherapy. Sure, my swollen lymph nodes disappeared a week after starting chemotherapy, and I haven't had any night sweats or itchy skin since around the same time, but these are somewhat qualitative measures of efficacy. Proving that the mass is shrinking with an x-ray, that's what feels good.
One thing I'm still unsure about is whether there will be any cancer (or, borrowing a term from some medical text I read, "residual mediastinal mass") left after chemotherapy. Stanford V calls for the use of radiation for any sites of disease that were bigger than 5cm at time of initial diagnosis. So I'll be getting the radiation regardless. It would definitely feel better if the radiation were just "to be sure" rather than "to finish the job", though.
When I was talking to Dr. Karamlou yesterday, I asked him if there was any chance that I could be cured right now. He said it was possible (this was before he had seen the x-ray results, I'm not sure if it would change his answer). In theory, at some point during the 12 weeks of chemotherapy, I will cross the line from being not cured to being cured. Unfortunately, with the current state of medicine today, there is no way of knowing exactly when that will happen.
Not that I'm complaining. I'm just glad that there's a cure at all. I do dream of a future when such medical precision will be possible. It would be pretty cool to stick your finger into a little box that analyzes your blood or DNA or whatever and prints out a report of exactly what's going on in your body. Treatments of any condition would be exactly tailored to each individual. Pretty far out there, but maybe some day.
Wired magazine had an interesting article entitled The End of Cancer (As We Know It) that discusses the first baby steps being taken toward this utopia. Notice the portacath surgery scar on the woman's chest in the picture. A few months ago, I wouldn't have even noticed it or known what it was for. Now I have a matching scar on my own chest, and it makes me identify on a very personal level with the article. I also feel a paradoxically intimate connection with the countless millions of other people who are anonymous to me, save that scar and what it represents.
- Tuesday, 16 December 2003 -- Chemotherapy #6; 50% done!
-
Today marks the halfway point in my chemotherapy treatment -- 50% done! The time has really flown by up until this point, and, as they say, it's all downhill from here.I had a horrible night's sleep (only about 2 hours) and was feeling pretty sick from sleep deprivation by the time I went into the office at 11:15. Lately, I have been wondering if it's sleep deprivation, rather than nausea, that is making me feel sick.
My vitals and bloodwork all turned out fine, as usual. I always have a little anxiety before seeing the results, a fear that some indicator or another is going to be horribly awry. The only borderline indicator is my hematocrit level (percentage of red blood cells), which is starting to get low. It's currently at 35%; they start thinking about doing blood transfusions if it gets to 30%. A single blood unit (one bag) raises hematocrit by 3 percentage points.
Before meeting with Dr. Karamlou, I met with a doctor named David Something, who is just starting his residency (for some reason, I can never remember last names of oncology fellows or residents...). I have seen him around the office a few times before; he is shadowing Dr. Karamlou and getting some hands-on oncology experience. He seems nice and competent, but obviously a little wet behind the ears compared to Dr. Karamlou. Aimee and I were thinking back to when we first met Dr. Karamlou and laughing at ourselves for worrying at the time that he might not have as much experience as other doctors we were considering. He seems like an old veteran now.
Even though "breaking in" a new doctor is a pain in the ass (on account of having to answer the same old questions over again), one thing I like is that the new doctor usually gives you a really thorough physical exam. The way I figure it, the more doctors that poke and prod you, the better the chances that nothing has been missed.
I have been freaking myself out lately because I can feel a lump just above my collarbone, in the "Spock nerve pinch area". I thought it was a lymph node that wasn't reacting to treatment. The new doctor assured me that it is most likely not a lymph node, but rather a tendon or something like that.
There is still a lot of fluid in both of my ears. It is clear fluid (not infected), so there really isn't much to do at this point but sit and wait for my rescheduled appointment with the ENT. Even though the fluid is in both ears, only my right ear hurts (just a slight, dull ache, not really that bad). I have been managing the situation with Sudafed, which seems to help a bit.
After the new guy was done, Dr. Karamlou came in to wrap things up. I mentioned to him that I have been getting a strong taste after meals whenever I burp (almost like I was about to vomit), and he said that I am getting acid reflux. He told me to stop taking the Pepcid completely and put me on a new drug, Nexium, which, in addition to being a cool purple pill, is a proton pump inhibitor.
Nexium is only taken once a day (versus twice a day for Pepcid), which hugely simplifies my life. Now, all of my essential drugs (Bactrim, Prednisone, Nexium, and Neupogen) are taken in the mornings and my non-essentials (daily multi vitamin, B12, Fibercon, Senna, Ativan, and Ambien) are taken in the evenings. Remembering to take my medications on time can be hugely stressful, so this is a big deal.
We also talked briefly about my insomnia, which is probably my number one complaint overall. I have been taking single doses of Ativan (1mg) and Ambien (5mg), from which I usually wake in the middle of the night after only 4 hours. He said that it is ok to double up my doses to 2mg and 10mg, respectively, in order to try to get a full 8 hours of sleep. I can also try taking 100mg of Thorazine, my hiccup medicine, although apparently this can cause painful erections that won't go away... yikes!
Dr. Karamlou seemed quite distressed when I told him about the severe nausea I had last week after treatment #5. He lightly chastised me for not calling the office right away so that they could do something about the situation, namely prescribing different drugs. He said that he was going to switch me over to a more potent anti-emetic for my odd week treatments from now on. My conventional wisdom throughout all of this has been that nausea is a given with chemotherapy and to just "grin and bear it", but I guess this isn't a given! We'll see...
My time in the chemo chair was extremely short this week, only one drip IV and one injection. It all happened so quickly that I forgot to collect my bloodwork statistics for my personal log (luckily I was able to get these the next day from Carol).
I wrapped up the day with a quick trip across the street to the hospital for a monthly progress check chest x-ray (required by the trial), and then went home and fell into a deep slumber.
- Sunday, 14 December 2003 -- After the fifth week; worst week yet
-
This past week was pretty bad. The worst yet so far in my treatment. From Tuesday through Saturday, I felt nauseated, tired, and unable to do anything but just ... sit ... and ... stare ... into ... space. To give one example of my typical state, Aimee came home Friday night to find me sitting in front of my computer, lights off, with my forehead pressed against the desk inertly. When you exist in the dark malaise of nausea, it doesn't matter where you rest, it all feels the same: Bad.
All week, I have persisted in the most horrible of purgatories: During the day, I longed for nightfall and the arms of Morpheus to take me away from my suffering, with the hopes that the next day would bring less nausea. Yet any respite was always short-lived, as I would inevitably wake in the middle of the night, restless for the first signs of daylight so that I could escape the eternal boredom of lying awake in bed at 4 o'clock in the morning.
Today I am finally feeling better. My right ear still hurts (I am going to try taking Sudafed all day to see if it is sinus-related) and I am pretty tired (after going to bed at 2:00 and waking up at 6:45), but the nausea is mostly gone, so I have no complaints!
- Thursday, 11 December 2003 -- Dr. Dierks; failed office visit
-
I was supposed to see Dr. Dierks today, but things didn't go as planned. I was feeling pretty nauseated today and not really looking forward to the office visit anyway, which almost assuredly would involve poking a fiber optic camera into my nose and throat.
Dr. Dierks has a trendy office on NW 18th Ave, but despite the Pottery Barn-esque setting, I didn't feel at ease there at all. The office has all of these signs like "$15 advance payment required for disability letters" and "No prescription refills on weekends, no exceptions!". I view these as red flags; if this is how they are going to treat you on petty issues, what sort of service are you going to get when it really counts?
After filling out my forms, the staff advised me that they wouldn't bill my insurance, Lumenos. I would have to pay $600 myself right then if I wanted to see the doctor, and then pursue reimbursement from Lumenos on my own. The staff wasn't all that pleasant about it either.
Having just felt the sharp end of Reasonable & Customary expense limits a few weeks ago, I asked them for the exact procedure billing codes so that I could call Lumenos and ask what the R&C limits for those procedures were.
Unfortunately, Lumenos was a bunch of e2es and basically said that they couldn't tell me what the R&C limits for the procedures were! Absolutely unbelievable. Here I am trying to control health care costs by proactively determining if the amount my doctor wants to charge is acceptable to the insurance company, and they tell me that the only way to find out is to submit a claim once I have the bill.
Dr. Dierks is in-network for Cigna (of course). Since I am switching to Cigna on January 1, I rescheduled my appointment for January 5. I don't meet with Dr. Nautiyal again until January 29, so I don't think the delay will cause any problems. Today's visit was a total wash, however -- frustrating and a huge waste of time!
- Wednesday, 10 December 2003 -- Chemotherapy #5, the day after
-
The actual chemotherapy procedure yesterday went pretty well, as usual. I am settled into my routine now, so I didn't really have any questions. This is the first week that I haven't met with Dr. Karamlou, so I headed straight to the chemo area and was done in about four hours. I watched Swordfish to pass the time, and also delved into the minutiae of the clinical trial protocol, which Carol had generously provided for me.
After the treatment, I was pretty tired, but was able to go home, eat a big dinner, watch the latest episode of "24", and get a decent night's sleep (compliments of Ativan).
Today, on the other hand, sucks. I feel terrible. I woke up with a raging headache, a metallic taste in my mouth, and some pretty nasty nausea. I don't feel like eating or drinking anything at all, as if it might make me throw up if I did. I took 1000mg of Tylenol for the headache, but it hasn't really done much.
I took Kytril and Compazine for the nausea, and I guess it's helping, but I still feel nauseated enough that I can't really do anything. I don't feel like watching TV, sitting, reading, computing, anything... I just sort of pace around the condo like a caged animal looking for something to do in my current condition...
- Monday, 8 December 2003 -- After the fourth week; end of the cycle 1
-
Today marks the end of my fourth full week of chemotherapy. The Stanford V protocol repeats in four-week cycles, so in theory I've been through everything that I'm going to be through. I can't shake this haunting feeling, though, that things are just going to slide slowly downhill from here, especially my tiredness level.
Before we get into that, here is a breakdown of each of the weeks of the cycle:
- Week 1: The worst week of the cycle due to the toxicity and sheer number of drugs delivered. Pretty severe nausea.
- Week 2: Not too bad, but feel pretty tired.
- Week 3: Second worst week of the cycle, on account of the back-to-back treatments on Tuesday and Wednesday. The drugs in this week have a long delivery time which makes for lengthy visits to the chemo ward.
- Week 4: Best week of the cycle. Not too many drugs. Actually feel normal at times.
So I am a little nervous about tomorrow, because I am going to be starting over on week one again (the worst week of the cycle). But things are probably going to be even worse this time since I don't have the fresh immune system like I had going into this four weeks ago. And I have to start up the daily Neupogen injections again.
I guess we'll see how it goes... I still have my hair and I haven't thrown up a single time yet, so I suppose I should count my blessings.
- Friday, 5 December 2003 -- Activity level
-
I have noticed a pattern emerging lately: I schedule all of my activities, including visits with friends, on my four healthiest days: Friday, Saturday, Sunday, and Monday. This makes for some pretty long days. The old me would have loved the constant activity, but the current me gets tired way too quickly for this to be sustainable.
My condo is like home base. If I am away from home base for more than an hour or two, I start to get uncomfortable. Part of this is physical: I get tired or sick really easily now, so it's nice to have all the amenities of home nearby should the need arise (think bathroom, couch, etc.). But there is a psychological component as well: Something about being at home is very comforting. I don't know if it's being able to take a nap whenever I want, or eat whatever I want, or mess around on the computer, tidy up, watch Tivo, warm up by the fire... but I pretty much like being at home all the time now.
Maybe it's the winter doldrums. Maybe I'm afraid of all the germs out there in the "big bad world". Maybe I like the feeling of complete control I have over my environment at home. Whatever it is, I realize that it's not healthy to become a total homebody. I think my couch has a butt-shaped impression in it from all the lounging around I've been doing lately.
I have decided that walking is going to be my new thing. Over the past few weeks, I have made a few short jaunts downtown for various errands, but I am going to start increasing my radius to farther destinations: A walk down to Pioneer Square for lunch or a quick game of chess with the homeless people. Or if I'm feeling ambitious, a lap around the waterfront (probably a good 5-7 miles).
- Tuesday, 2 December 2003 -- Chemotherapy #4; one-third done
-
Last week's back-to-back chemo treatments really took their toll on me in terms of nausea and morale: I started to question whether I could handle nine more weeks of psychological seesawing between sick and healthy. Luckily, this week's treatment was the easiest one that I've had to-date. My spirits have buoyed. I am also officially 1/3 done with my chemo treatment -- woo-hoo!
I started off with a brief physical examination with Dr. Karamlou. I have been meeting with him every chemo treatment, but after this week, I will only see him for a consultation every other treatment. This makes sense to me as I am starting to settle into my routine and won't really have many questions for him.
I really didn't have any serious issues, but I enumerated the previous week's ailments for him, including:
- The worst nausea yet.
- Tingling in the first two fingers on both hands. If it gets any worse, they will have to reduce my dose of the drug that is causing this (Velban, I think).
- Extreme fatigue for the first 2-3 days after chemo (an indication that my blood counts are dropping).
- Extreme insomnia after that.
- Occasional hot flashes and bone marrow pain. Caused by extreme white blood cell production.
My ear ache from last time was still present. He took a look inside and said that it wasn't infected, but noted that something was bulging from my inner ear, probably fluid. I will be meeting with the ENC specialist, Dr. Dierks, next week, so I can ask him about it then.
I also learned that I will have to take the Neupogen shots every other week for the rest of my treatment. Aye-yah! That's 20 more shots. Luckily I still have plenty of room in my red biohazard container. I had thought that they would take my blood counts each week and only give me the shots if necessary, but Dr. Karamlou said that history has proven that patients whose counts have dropped once will drop again when subjected to the same drugs.
On the bright side, the Neupogen shots really work! My neutrophils rocketed from 600 to 11,800 and my white blood cells went from 2,200 to 16,200. The levels that I'm at now are way higher than normal. In keeping with the ping-pong theme of chemotherapy, I went from being almost immuno-compromised to immuno-overload!
The chemo ward was the fullest I've ever seen it; Nancy really had her hands full juggling all of the patients. One woman was receiving a blood transfusion, the dark red IV bag hanging above her chair a dead giveaway. A man beside her was hooked up to one of the largest drip bags I've seen yet, probably a 3-hour drip from the looks of it. Another woman was sleeping/resting next to him, wrapped snuggly in some nice blankets that the office keeps handy in case we get cold. A few other patients shuffled in and out during my stay for miscellaneous bloodwork, but they didn't get any chemo.
Luckily for me, this week's treatment was mercifully short, only two small drip bags and one push injection. We were out of there pretty quickly. A nice change from previous weeks. I barely had time to finish my weekly trials interview with Carol before it was time to head out.
One final note: As you can tell from the daily photos, my hair is still here. Dr. Karamlou seems to think it's a sure bet that I will lose most of it, calling Etoposide (one of the chemo drugs) a "hair killer". If it's going to happen, I want to get it over with. My hair is getting long and I may need a hair cut soon. And I'll be pissed if I shell out $12 for a hair cut and then have all of my hair fall out the next day :-)
- Monday, 1 December 2003 -- Dentist visit; Dr. Dutro
-
I had panoramic x-rays taken and fluoride tray molds made at my dentist's (Dr. Dutro) today. Dr. Nautiyal recommended that I complete both of these precautions before my radiation treatment begins in February. The idea is to get my mouth as strong as possible beforehand to minimize any treatment-related problems or side effects. It felt really good to be getting this taken care of well in advance, rather than rushing around at the last minute like I have been up until now.
When the assistant was checking my chart, she remarked, "there must be a mistake, it says here that you're getting pano x-rays done." Apparently these are only taken before pulling wisdom teeth or for really old patients. This sort of response happens to me a lot when dealing with medical professionals who just see a healthy 30-year-old man in front of them.
The pano x-ray machine is a great example of the refinement and elegance that are possible with mature diagnostic procedures: You position your head in a clasp and bite down on a plastic tab. The machine then rotates around your head, ultimately producing a single, long x-ray film with all of your teeth displayed linearly. Even though it produces an x-ray of the entire mouth, the machine produces way less radiation than those little mini x-rays that only show a few teeth.
Making the tray molds was pretty straightforward and involved copious quantities of bland flavored goo. It is basically the same process used for making teeth whitening trays. These will be ready in a few weeks, along with the fluoride treatment paste. Dr. Dutro generously cut me a deal for all of this, charging me only $200 for making the trays and the fluoride to go with it (3-6 month supply), well below the regular price. I think he felt bad for me because of what I'm going through and also because my insurance probably won't pay for this.
Dr. Dutro reviewed my x-rays, physically examined my mouth, and said everything looks fine. He recommended a routine cleaning if possible during the rest period between chemo and radiation (I am overdue for one, but cannot get one during chemotherapy treatments).
Dr. Dutro also said that he had had a lengthy phone conversation with Dr. Nautiyal about my case and was extremely impressed with Dr. Nautiyal, calling him the best oncologist that he has ever worked with. In particular, I think he was impressed with the emphasis that Dr. Nautiyal places on minimizing collateral damage as much as possible through the use of thorough dental inspections, fluoride trays, masks, etc. Dr. Dutro's emphatic support further cemented the already high esteem that I hold Dr. Nautiyal in.
During my entire visit, I could feel a strong sense of empathy coming from Dr. Dutro; my guess is that he isn.t often involved in the care of seriously ill patients. From this, and the fact that he has always given me excellent dental care over the past seven years, I can wholeheartedly recommend Dr. Dutro as a caring and proficient dentist (if you're ever in the market for a dentist).
- Saturday, 29 November 2003 -- Quotes
-
Excerpts from Taking Time, National Cancer Institute, NIH Publication No. 92-2059:
The Years After
That pretty much sums it up. Or, as Rush succinctly puts it in Dreamline:Cancer is not something anyone forgets. Anxieties remain as active treatment ceases and the waiting stage begins. A cold or a cramp may be cause for panic. As 6-month or annual checkups approach, you swing between hope and anxiety. As you wait for the mystical 5-year or 10-year point, you might feel more anxious rather than more secure. [...]
Cancer might rob you of that blissful ignorance that once led you to believe that tomorrow stretched forever. In exchange, you are granted the vision to see each today as precious, a gift to be used wisely and richly. No one can take that away.
When we are young
Wandering the face of the Earth
Wondering what our dreams might be worth
Learning that we're only immortal
For a limited time - Thursday, 27 November 2003 -- First injection; Thanksgiving
-
The injections aren't too bad. We take the syringe out of the fridge and let it warm up for about 30 minutes first since apparently it hurts less this way. The needle is pretty small (29 gauge) and, according to Aimee, "goes in very easily, like your flesh is nothing." The initial jab isn't very painful, but it does hurt when the medicine is being pushed in. The whole process takes about a minute. Our instruction sheet recommends the stomach as the ideal injection location, but I much prefer the back of my arm.
Still feeling pretty sick today. I did manage to eat Thanksgiving dinner with Aimee's relatives, which was nice. I stuffed myself thoroughly and officially registered my highest weight since I started treatment.
- Wednesday, 26 November 2003 -- Chemotherapy treatment #3 (part 2)
-
Today was the worst chemo day yet. I woke up feeling pretty nauseated, popped a Kytril (these cost $41 each, by the way), and headed over to the office for part two of my treatment. I couldn't help but feel demoralized as I entered the office for the second time in under 24 hours. Overall, it went "ok", but for the first time ever, I felt nauseated while receiving the drugs, enough so that I couldn't do anything but sit there and stare vapidly into space. It also really sucked having my port accessed two days in a row.
On the bright side, I slept like a log last night. I ate a small dinner around 6pm, took a four hour nap, and then went to bed and slept through until 8am. On the down side, I feel extremely listless -- I don't feel like doing anything at all, and I'm tired, but I don't want to sleep any more either. I don't know what's worse: Being wired on steroids and not wanting to sleep or being in this lethargic undead state.
I'm looking forward to Thanksgiving tomorrow. If the pattern of previous weeks persists, my appetite should return and I should start feeling less nauseated.
- Tuesday, 25 November 2003 -- Chemotherapy treatment #3 (part 1)
-
Every week, I get a complete blood count (CBC) before my chemotherapy treatment begins. This week, my neutrophil (ANC) levels were really low, only 600 per mL (normal is 1400-6500), which means that my ability to fight off infections is greatly reduced. If it had been any lower, I would have had to skip treatment entirely this week. Instead, I received only 65% the normal dose of chemo drugs in order to give my immune system a chance to recover.Because my white blood counts are so low, I now have to get daily injections of Neupogen (PDF), a Granulocyte-Colony Stimulating Factor (G-CSF) that will force my bone marrow to produce more white blood cells. These shots can be self-administered, but having somebody else do it is recommended. And the lucky winner is ... Aimee! Nancy trained her on how to give the injections: The drug comes in single-use, pre-measured syringes that are stored in the refrigerator. The injection is given subcutaneously (underneath the skin), just like insulin injections for diabetics. I even received my very own red biohazard container for used "sharps".
Dr. Karamlou reviewed my symptoms from the previous week:
- Ear ache. He verified that I have an ear infection and prescribed antibiotics to make sure it gets taken care of.
- Extreme lower back pain. I started feeling intense (but intermittent) pains above my pelvis yesterday. I had wondered if I had pulled my back somehow, but Dr. Karamlou is pretty confident that it was caused by my bone marrow in my pelvis going into overdrive to produce white blood cells. He said that the Neupogen injections will likely cause more of the same type of bone pain.
- Insomnia. He prescribed a different drug, Ambien, to help with my insomnia. While sleeping pills can be addictive, getting adequate sleep is far more important for me right now, so I am to take as many as I need to get good rest. This drug replaces the Ativan that I was using previously.
- Racing heart rate. This is an unavoidable side effect of the Prednisone. I shouldn't worry about it unless I feel discomfort or have another symptom (i.e., fever).
I received the "week 3" chemo drugs this time, which is the same as week 1, minus Cytoxan, plus VP-16. Stanford V is a very complicated regimen; it helps to understand that it is actually a 4-week cycle that repeats for 3 cycles. I found this schedule page helpful in understanding everything.
I watched "Serendipity" on the portable DVD player during treatment. It was a perfect choice, nice and lightweight, easy to digest.
The chemo treatments are starting to get to me. Stanford V is a very intense protocol. With ABVD, I would have had two weeks between treatments, but with Stanford, they come relentlessly, week after week. Usually, I am just starting to feel "normal" by Monday night, and then it's back to being sick again...
- Monday, 24 November 2003 -- Dietician
-
I met with the dietician today. Their office appears to be set up predominantly for educating diabetics, but they take skinny cancer patients too. I already had a pretty good understanding of nutrition, so I didn't learn anything groundbreaking, but it was nice to get the official stamp of approval for my diet.
My body mass index is less than 20, which means that my body is not as resilient as it needs to be for treatment. Thus, I need to eat, eat, eat, until my weight is back to at least 150. Here's the best part: The extra calories can come from any source. Pepsi, donuts, cheese, McDonald's, whatever it takes. I'm supposed to reverse all of the standard dieting tips. Meal right before bed time? Do it! Water? Drink juice or soda instead. Salads, soups, fruit, and vegetables? Try some cheese, nuts, oils, butter, or candy. Microwave chicken pot pie with 65g of saturated fat? No problem!
Aimee had been keeping a food log for me over the last few weeks, which I showed to her. She said my diet was fine, but too healthy and lean. I need more calorie dense foods. The reasoning is that since I'm underweight and it's only for a few months, it's ok to depart from the healthy eating rules that govern our obese society.
This is great!
I also asked her about some anecdotal advice I've received regarding foods that cancer patients should avoid, like sugar and cheese. She said she had never heard anything about this and to stick with the reputable sources, like the USRDA and the National Cancer Institute. She recommended a daily multivitamin as scientific studies have proven that they work, but any other supplements are probably a waste of time (and maybe even dangerous). Sounds good to me.
I celebrated my new diet by heading to McDonald's after the meeting for a McGriddle sandwich and 32oz. Dr. Pepper. Life is good.
- Sunday, 23 November 2003 -- After the second week; insomnia; ear infection; sore throat
-
None of my hair has fallen out yet. And, like last week, the nausea and general ickiness were gone by Friday night/Saturday morning. But the Prednisone is taking its toll on my body. I have persistent insomnia and have been getting only 4 hours sleep a night for the past week. On days that I take the steroids, my resting heart rate is above 100 bpm and I feel totally wired. On days that I don't take them, my heart is not that high (only 10-15 bpm above normal). Unfortunately, although I feel extremely tired, I cannot sleep in late or take a nap to get caught up on my sleep deprivation. My body simply refuses to sleep!
I also think I may have an ear infection. My right ear has been aching moderately since Friday. I called the on-call nurse on Saturday and she said not to worry about it unless I had a fever as well, which I don't have. It isn't painful enough to prevent me from sleeping, but it is annoying.
And a new symptom: Sore mouth and throat. It hadn't occurred to me until one of Dr. Nautiyal's nurses mentioned it, but the rapidly dividing cells that chemotherapy kills includes those in the lining of the mouth and gut. The nurse looked inside my mouth and said that she could see lots of tiny white spots, which I guess means that my mouth is starting to slough off cells. It hasn't affected my ability to eat (thankfully!). I gargle with a water-salt-baking soda solution several times that restores my mouth's pH-balance and alleviates the symptoms.
- Saturday, 22 November 2003 - Body Surface Area Dosage
-
For some time now, I have been wondering what the "/m2" (per meter squared) listed next to the drug dosages on the chemotherapy cocktail recipes means (see the ABVD or Stanford V recipes to see what I'm talking about). Thanks to this explanation of the Body Surface Area (BSA), I now know. It's amazing how much detailed healthcare knowledge is on the Internet. This system allows the drugs to be listed in standardized form and then adjusted based on the size of the person. Apparently your body's surface area is a much better parameter to use than your weight (although they must be somewhat related).
Taking my height and weight, I calculated my BSA = sqrt(71*142/3131) = 1.79.
I then figured out what my doses for each of the Stanford V drugs should be:
Drug Protocol dose My dose Doxorubicin 25mg/m2 44.86mg Vinblastine 6mg/m2 10.77mg Cytoxan 650mg/m2 1166mg Vincristine 1.4mg/m2 (2mg max) 2.51mg (2mg max) Bleomycin 5u/m2 8.97u VP-16 60mg/m2 107.66mg (week 3 only) Prednisone 40mg/m2 71.78mg Each time Nancy hooks up a new IV drip bag, I have Aimee get up and read the label to me to make sure that the drug and dosage are correct. One of my biggest fears is that I'll get the wrong drug or the wrong dose. With an IV, there isn't any messing around -- it goes straight to your entire body in a few seconds. If the wrong thing goes in, it isn't coming out!
- Friday, 21 November 2003 -- Insurance woes
-
I was pretty stressed out last night about insurance. My insurance plan, Lumenos, sends me a statement whenever they process a claim. Normally I look forward to these statements as they give me an idea for how much my treatment is costing, but my most recent batch of bills totally freaked me out. Lumenos is a new insurance company that my company made available to us this year. For a relatively healthy person, it seemed like a nice plan because it gives you a flexible spending allowance and (supposedly) freedom from provider networks. So I switched. But there's nothing like a bunch of serious medical expenses to test out the system. Here's what happened:
Lumenos paid the first $1300 of my medical expenses this year. Then, I paid the next $700 out-of-pocket, a period Lumenos refers to as "the bridge". Once the bridge was paid, I paid 10% coinsurance on the next $3000 of expenses, after which Lumenos was supposed to start paying 100% again. This sounds complicated, but it basically means that my cumulative annual out-of-pocket expenses should have been $1000 max. I reached this limit back when I had the neck surgery biopsy. This is more money than I would have spent out-of-pocket on my old plan (Cigna), but I consoled myself that at least I didn't have to mess with any of that in-network or referrals stuff.
As it turns out, Lumenos does have "preferred providers", which is essentially the same thing as a network. If you stay in-network, they pay the bill 100%. If you go out-of-network, they still pay the bill 100%, but only up to a maximum "reasonable and customary" amount. Any amount over the R&C limit is passed on directly to me. The $1000 annual maximum doesn't apply. Aaaaaaaaaaaaahhhhhh! This exposes me to unlimited expense liability.
Due to a mistake with Dr. Karamlou's tax id number, they were billing him as out-of-network. And tons of expenses were ringing up beyond the R&C limit. After a bunch of phone calls, the tax id number is fixed and they are going to reprocess all of his bills. But Dr. Khaki is out-of-network. And Dr. Nautiyal isn't in there either. What a mess. It's going to take a lot of phone work to straighten this out. And I'm basically at the mercy of the doctors and their offices -- if they decide that they don't want to join the Lumenos network, I'm toast.
Every doctor I've seen is in-network for Cigna, my old insurance company. Cigna has a $10 copay for doctor visits and a $5-16 copay for prescriptions, which is obviously a much better system if you are going to be getting a lot of health care. So I'm switching back first thing next year. In retrospect, I wish I had stayed with Cigna, but that's the power of hindsight.
The moral of the story for me is that point-of-service or network health plans are a good thing. In Portland, the doctors are all on Cigna and they know to keep you in-network if they refer you to another doctor. They also make sure to send any lab work or diagnostic tests to in-network providers. On a new insurance plan like Lumenos, you could get into trouble because the preferred provider directory is not as large and the expenses might not be covered past the R&C limit. Caveat emptor!
[Update 23 November: I wanted to add that I am not complaining TOO much here. My company has pretty darn good health coverage overall. And I really like the consumer-driven philosophy behind Lumenos, the attitude of their employees, and what they are trying to do. Somebody has to get health care costs under control, and this is a good start. For my needs now, however, I think Cigna is far and away going to be the better plan for me moving forward.]
- Thursday, 20 November 2003 -- Radiation oncologist, Dr. Nautiyal
-
I went to see my radiation oncologist, Dr. Nautiyal, for the first time today. Due to a scheduling mix-up, we had to wait quite a while to see him, but it was worth the wait: Dr. Nautiyal is one of the best doctors I've ever met! He is extremely thorough, takes his time, listens attentively to what you have to say, explains the complete history of your particular disease and how treatment for that disease has evolved over time, and spends as much time as necessary to ensure that all of your questions are answered. I had prepared a list of questions for him ahead of time, as I do every time I see any doctor, but by the end of our meeting, he had answered them all! I suppose doctor's visits are like job interviews, and you're supposed to always ask at least one question, but I couldn't think of any! Office visit score: A++. The office visit went so well, that I have absolutely no desire to get a second opinion.
He had me go over in detail the events leading up to my diagnosis and then proceeded to give me an extremely comprehensive physical examination. He started by testing my reflexes, limb strength and flexibility, and all of the sorts of things you would expect in any physical. Then he started feeling for lymph nodes, including areas where no other doctor has gone before (like my legs). He said that he couldn't feel any lymph nodes, meaning that they are all less than 1cm. The chemo is working!
During the exam, I made a few "throat clearing sounds", as I often do, and he asked me about those. I told him that I've had the problem for at least 3 years. He wanted to take a look inside for any obvious problems, so we went into another room where he jammed a fiber-optic tube in my nose and down my throat. This was uncomfortable, but not painful, thanks to the liberal use of some numbing spray. He said he really didn't see anything, although there was a deposit of some extra tissue in an area directly behind my nose called the nasal pharynx. He is going to refer me to a highly regarded ear-nose-and-throat specialist (Dr. Dierks) for another opinion. He thinks the tissue is benign, but wants to be on the safe side.
I thought I knew pretty much all that there was to know about Hodgkin's, but Dr. Nautiyal surprised me with a lot of information I didn't know about how the treatment for the disease has evolved over the years. For instance, Hodgkin's research today is advanced primarily by pediatric oncologists. With children, the goal is always to reduce the toxicity as much as possible, and any advances eventually trickle over to the adults. I won't go into all of the history that we talked about, but my overall take-away is that chemotherapy plus radiation is the most historically proven way of treating Hodgkin's and making sure it doesn't come back.
Next, we discussed my treatment, which will most likely be 36 Gy (sometimes referred to as 3600cGy or 3600 rads) of involved field radiation to whatever is left of the original 7.5cm mass in my mediastinum. I say "whatever is left" because it is expected that the mass will have shrunk considerably by the end of my chemotherapy treatment. The trial protocol is quite specific in the radiation therapy that I am to receive, but Dr. Nautiyal assured me that he would not hesitate to contact the trial organizers if he felt that I needed different treatment than what was suggested by the trial rules.
Some of the possible side effects of my radiation are listed below, in order of decreasing likelihood:
- Hypothyroidism. The thyroid gland is smack dab in the middle of the area that is going to be irradiated. There is a 15% chance that my thyroid will be destroyed by the radiation, which will lead to a condition known as hypothyroidism (under-production of thyroid hormone). This would suck, but would not be the end of the world; if this happened, I would have to take a pill every day for the rest of my life to replace the missing thyroid hormones.
- Saliva glands. The saliva glands are also close to the area being treated. There is a small chance, although not as great as hypothyroidism, that my saliva production will be permanently reduced, resulting in "dry mouth". In addition to lowering the bacterial resistance of the mouth, this can drastically change the taste of food.
- Heart and lung problems. My radiation will be above the heart and lungs, so there is very low risk of anything happening to these vital organs. I think I will be getting a protective shield to guard against stray radiation to this area.
- Dental problems. Radiation to the mouth can result in all of your teeth falling out! While this is very unlikely in my case, Dr. Nautiyal is going to work with my dentist, Dr. Dutro, to have some fluoride trays made. I am not sure how the trays are used, but they will decrease the probability of any nerve damage to my teeth. I will also be fitted with a protective mask that will shield my mouth and face from the radiation.
Dr. Nautiyal said that the amount of radiation I'm getting (3600 cGy) is a relatively low dose by oncology standards (lung cancer patients receive over 7000 cGy, for instance; serious adverse side affects usually don't start until at least 4000 cGy). The new IMRT radiation technique is really not applicable in my case, since it is intended for patients who are going to be receiving much higher doses of radiation. Additionally, there is no clinical data yet proving the efficacy of IMRT for treating Hodgkin's. Incidentally, Dr. Nautiyal is the only physician qualified to do IMRT at Good Samaritan hospital.
It's nice to start planning this stuff a full two months ahead of time so that it will all be ready when February arrives. I'm sure I'll have a lot more details about the radiation technology and procedure at that time.
- Wednesday, 19 November 2003 -- The day after chemo #2
-
Today has pretty much sucked. I'm afflicted with your basic nausea. Can't eat. Can't sleep (the steroids have me too wired). Can't think straight for more than 5 minutes. I'm not in that much pain, just that annoying flu feeling. I feel like a caged rat.
On an absolute scale, it's probably not as bad as last week, but it's hitting me extra hard because I was just starting to feel normal again over the weekend. Oh, to run in Elysian Fields, only to have it yanked away as each chemo cycle begins anew...
I got a call from Dr. Segal asking how I was feeling and to see which treatment I had decided on. I had sent him a card last week letting him know that I was staying with Dr. Karamlou, so I hadn't expected to hear from him again. It was a nice surprise. Dr. Segal is a genuinely nice guy. He said that he had a "good feeling about my chances". I really appreciated his taking the time to call and check in on me.
Also, it snowed in Portland this morning for a couple of hours! Big puffy white flakes that floated gently to the ground, and then melted away, their ephemeral journey complete. Watching the snow fall made me feel a lot better. The whole scene was surreal, especially amidst all of the colorful foliage of fall. I felt as if the whole thing was happening solely for my benefit, to celebrate my getting better, even though I feel crummy now.
- Tuesday, 18 November 2003 -- Chemotherapy treatment #2
-
Chemotherapy treatment 2 bloodwork statistics
Heart rate: 68, BP: 138/80
WBC: 5.3k, HGB 13.4, HCT 40.6, PLT 209k, ANC 2.6k, RBC 4.8M
Summary: Counts are dropping; borderline on HGB and HCTLast week, I promised a description of what these numbers mean, so here goes:
Indicator Unit Normal range What it means WBC count/uL 4.5k - 10k Number of white blood cells per uL of blood. Measures body's overall ability to fight infection. ANC count/mL 1.4k - 6.5k Absolute Neutrophic Count. Number of neutrophils per mL of blood. Neutrophils are the body's primary defense against bacterial infections. HGB g/dL 13.8 - 17.2 Measures total amount of hemoglobin per dL of blood. Hemoglobin carries oxygen in the blood; a low count means I won't have much energy. HCT % 40.7% - 50.3% Hematocrit. Measures percent of blood that is red blood cells. Low levels mean decreased energy levels. HGB and HCT results are interpreted together. PLT count/uL 150k - 400k Total number of platelets per uL of blood. Platelets are responsible for blood clotting; too few increases the risk of bleeding. If my count goes below 50-100k, I can't floss my teeth or use a razor. RBC count/uL 4.7M - 6.1M Total number of red blood cells per uL of blood. These cells live about 120 days and thus are not affected as much until the later stages of chemotherapy. Today was chemotherapy treatment #2. I met with Dr. Karamlou first and went over the symptoms I've been having. Everything seemed acceptable so he didn't change any of my medications. He did say that Ativan can be habit forming, and that that the body will eventually adapt if you use it to much (thereby nullifying the benefit of the drug).
My biggest fear during the first week was that I would be "chemo resistant" (a small percentage of people have uber-immune systems that fight off the drugs.) I certainly felt sick enough, and I often feel a dull ache in my lymph nodes that indicates a siege is underway, but the doubt still lingers in my mind. Dr. Karamlou did a physical examination of the lymph nodes in my neck and armpits and remarked that they had already shrunken quite a bit. I guess I must have gotten used to my appearance from seeing myself in the mirror everyday, because I hadn't noticed any changes at all. This news buoyed my spirits a bit.
Nancy had already been in to prep my port and withdraw the requisite blood samples, so I was primed and ready for treatment. The treatment area was a lot more crowded than the last time and my favorite chair with the view was already taken. I had to take a lesser chair without a view, but I consoled myself that the leaves had all fallen off the trees anyway so it didn't matter that much. The woman in my favorite chair was slumbering soundly as if she had been there for some time, and, based on the amount of medicine left in her IV bag, was going to be there for quite a while longer. Seeing the other treatments that patients get reminds me that, as horrible as what I have is, I am not nearly as bad off as some. My chemotherapy "drip time" is usually only an hour or so a week, compared with some cancers that can be 5 hours every weekday!
This was my first "even week" treatment, which is not immunosuppressive and is supposed to be "easier" than the odd week treatments. The drugs du jour were:
- Vincristine: An anti-cancer drug that stops cells from dividing. Like all chemotherapy drugs, it causes nausea and hair loss. It is also known for causing severe constipation. I stocked up on Colace, Senekot, and Fibercon tablets as a preventative measure. These are all over-the-counter medicines. (Meaning I had to pay for them myself. Strangely, I actually prefer prescriptions now, since they are 100% free to me as I have already met my annual insurance out-of-pocket maximum.)
- Bleomycin: An anti-cancer drug that stops cell growth and division. Bleo can cause permanent lung damage if the total lifetime dosage exceeds 600u/m2. Luckily my total dosage for my entire treatment will be 30u/m2. Some people get a fever or chills for a few hours afterwards, but this didn't happen to me.
Carol stopped by and gave me a nice calendar of my office visits, detailing which treatment I would get on which day, as well as any additional tests or other trial requirements that had to be met for that day. She also gave a copy of this to Dr. Karamlou and Nancy, which made me feel better. The trial and treatment are just complicated enough that it's nice to have it all clearly written down so that no mistakes are made.
Aimee picked up a turkey panini sandwich from La Buca and I wolfed it down during treatment. Even though the total time getting the chemo drugs is not that long, the total office visits have been running about 3-4 hours from arrival to departure, so eating during the visit is a must. I do not get nauseated during treatment or have any ill effects (those come later), so eating is no problem. I noticed that nobody else ever eats, however, which is a shame, because the office has unlimited free candy, granola bars, and juices. I need to work on them to install a Pepsi machine too.
I was given a prescription to stop hiccups, but they didn't happen like last time. I was told that I didn't need to take the Kytril medication, which is a fancy drug that comes in its own box (2 pills per box). I haven't seen the bill yet, but it must be an expensive chemotherapy-specific drug. In any event, it seems that my treatments this week won't require the use of the Kytril, which is probably a good thing since it caused a pounding headache the last time I took it.
We went home and I fell into a deep sleep on the couch for several hours. I woke up feeling queasy to my stomach. I took some Compazine (and later an Ativan before bedtime), but still wasn't able to eat very much. I started to feel like I might throw up, so I retired to the couch and watched TV for the rest of the evening, and then went to bed. Thankfully, the Ativan had kicked in and I was able to get to sleep relatively easily.
- Sunday, 16 November 2003 -- After the first week
-
When I read stuff like this, I am really glad that I am on the Stanford V treatment. (Read the RESULTS section near the middle.)
The most common question I get nowadays is "how are you feeling?" The short answer, all things considered, is that I can't complain. I have come nowhere near my imagined worst case scenario, which is that of being hunched over the toilet in a permanent nauseated state, unable to sleep, eat, or move.
Instead, I experience mostly tiredness, along with the side effects of being under siege from a dozen active drugs in my system. It's a lot like having a bad cold or the flu, except that every time something hurts or I feel funny, I get to worry about whether it is an expected side effect from the chemotherapy or the anti-nausea drugs, a known lymphoma symptom, something new that I should report to the doctor, or (most of the time) just a random body ache that I should ignore.
I often visualize the drugs as a sort of fiery orb inside me. When the drugs are controlling each other, the orb is held in check and all is normal. Every now and then, one of the drugs will erupt inside the orb, a crack will appear, and some side effects will shoot out before the other drugs get it under control again. If one of the drugs were to fail in this balance of power, the whole orb would probably blow up in cataclysmic furor (and take me with it).
With that said, here are most of the symptoms that my body and I have been learning about for the past week:
- Pounding headaches. I really only had this the day after my first treatment. It was readily dispatched with some Tylenol. It was probably my body saying, "What the hell did you just do to me?!"
- Hiccups. Very annoying for a day and a half, and then they mysteriously went away. None of the tricks worked (breathing into bag, drinking water upside down, etc.).
- Torpidity. I have been getting decent sleep at night (with one notable exception below), but I find myself getting extremely tired as the day goes on, especially in the late afternoon and early evening. I literally can do nothing until I take a 2-3 hour nap. I usually bounce back around dinner time.
- Fingertip tingling. The tips of some of my fingers have been tingling and/or numb since Thursday. It isn't really painful or annoying... just worrisome! A sign that powerful stuff is underway inside my body. Nevertheless, it is an expected side affect of both Adriamycin and Velban.
- Constipation. The nurse told me to call if I didn't have a bowel movement after 3 days. I've come close to that limit, but haven't exceeded it yet. I am drinking tons of water and snarfing down fibrous "colon blow" foods by the mouthful, but my bowels don't even flinch. Apparently the new chemo drugs coming up next week will only aggravate the situation... oh goody!
- Metallic taste. One of the side effects that often appears out of nowhere "from the orb" is a strange metallic taste in my mouth, usually at the back of the throat or the tip of the tongue. It hasn't affected my appetite and usually goes away quickly enough. It's just weird.
- Insomnia. I've been getting pretty good sleep all week, but the Prednisone (steroids) finally caught up with me last night. After reading in bed for hours, and then sitting in the dark fidgeting for hours more, I finally just got up and started downloading Britney Spears MP3s on my computer (I'll let you decide if this was a sign of my utter desperation or an indication of my poor musical tastes). Around 4:30am I admitted defeated and took an Ativan, which finally made me go to sleep. (My philosophy has been to take as few meds as possible. In this case, however, I will probably start taking an Ativan in the evening whenever I take Prednisone in the morning, which is every other day.)
The good news is that for most of today, I've felt pretty normal! Other Hodgkin's patients taking biweekly chemotherapy regimens (like ABVD) have told me that they usually only feel really sick for the first 5 days after each treatment, which seems to agree perfectly with what I'm feeling. Of course, I am getting weekly treatments, so this coming week will be a big prognosticator for what's to come.
- 12 November 2003, Wednesday -- Chemo: The day after
-
I had a fairly good night's sleep, except for the fact that I had to get up at 4am for a mandatory bathroom break. It is imperative to urinate at least once during the night so that toxic anti-cancer drugs (and hopefully lots of recently deceased cancer cells too!) don't pool in my kidneys.
I woke up with a pounding headache (probably a side effect of the Kytril). I'm not allowed to take aspirin or ibuprofen, so Aimee called Nancy (the chemo nurse) and asked what to do. She said 1000mg of Tylenol was safe, and it seemed to mute the pain quite a bit.
The rest of the day, I have had a persistent hiccup along with a general malaise, similar to what you would get with a cold or flu, but without the congestion, runny nose, or head fogginess. Mostly a lack of energy and some head wooziness mixed in with a restless desire to go out and enjoy the crystal clear blue sky perfect fall day outside.
I am going to try to go into work tomorrow for at least a little bit. I can't drive while I'm taking some of these drugs, so I am going to brave my way on the train. I normally am a hard-core train commuter to work, but I am worried about being locked in to a 30-45 minute train commute if I should suddently start feeling ill. I guess I'll pack a plastic bag to throw up in just in case.
- 11 November 2003, Tuesday -- Chemotherapy treatment #1; lots of prescription drugs
-
Chemotherapy treatment 1 bloodwork statistics
Weight: 142, Heart rate: 80, BP: 130/80
WBC: 7.3k, HGB 15.1, HCT 43.0, PLT 222k, ANC 4.8k, RBC 5.2m
Summary: Everything normal!
(More on what all this means some other day when I have more time...)(This is going to be a long entry. Bear with me -- a lot happened today.)
We showed up at the office at 11:15 and met first with Dr. Karamlou. He briefly went over the chief side effects of the drugs used by Stanford V (much of which I knew from reading the consent form). He stressed several situations in which I should call him immediately, 24-hours a day. If I get: fever above 100.5; bowel obstruction or abdominal pain; chills; or tingling in my hands or feet (indicating nerve damage). Or, more generally, if I feel anything weird, I'm supposed to call them immediately. I'm in the world of hard core biochemistry now, where the smallest perturbance warrants attention.
I also asked him about some of the diet advice that my militant vegan/vegetarian/naturopathic friends have been giving me (for example, don't eat sugar, cheese, or caffeine). He said there's no medical proof that any of that advice makes a difference and advised me to eat whatever I want. The most important thing is staying nourished and hydrated. Since my insurance covers it, I asked for a referral to a licensed dietician who could help me form a good chemotherapy diet. He agreed that this was a good idea and I'll be meeting with her in a few weeks.
Lastly, he referred me to a radiation oncologist to start discussing the next phase of my treatment, the irradiation of my mediastinal region. That's right folks, I've just barely begun chemotherapy and it's already time to start planning the radiotherapy.
Next up, my first chemotherapy treatment ever:
I met Nancy, the oncology nurse who oversees the chemo administration area. I'm glad Nancy's my nurse; she is friendly, caring, capable (as I would learn while watching her perform her myriad tasks), and always happy to answer any question I had about the minutia of chemotherapy treatment.
A brief description of the office: There are ten or so leather La-Z-Boys, each with lots of comfy pillows and candy nearby. Lots of free drinks like orange juice and tea are available in the kitchen. The nurse's station is in the center of the room, and she periodically makes the rounds to check on the patients, inject the next drug, etc. Just like flight attendants taking care of passengers on the plane. They even have portable DVD players and a nice collection of recent DVDs releases available (unlike the airlines, they're free here).
Aimee was there to keep me company, but the other two patients were alone. I was much more comfortable getting my treatment here than in any of the other offices that I've seen. The other offices were packed full, every chair occupied, with 4 or 5 nurses running around keeping everything running. Very chaotic. I much preferred the calm, quiet setting of my treatment. From my comfy chair, I had an extremely soothing view of NW 22nd Ave and all its trees, swaying gently in the wind, glorious in their fall splendor. The occasional pedestrian would saunter by as well, blissfully unaware, I'm sure, of the precious gift they have in their health.
Carol, my trials nurse, arrived with about 20 blood sample vials that needed filling for various tests. Nancy expressed surprise at the number of vials -- you know it's a lot when a battle-hardened chemo nurse speaks out!
Nancy started by tapping into my chest port catheter, the first time it's been used. She swabbed the entire area with betadine, and then blasted me for a few seconds with some super cold aerosol spray that numbed the area. Then she popped in the needle, which hurt for a millisecond and then didn't cause me any trouble for the rest of the visit. I am so glad that I got the portacath, as it is clearly going to make this whole process a lot easier on me. By comparison, the Red Cross blood donation prick is far worse than the one I received for my portacath.
Once the portacath was in, it was smooth sailing the rest of the day. Nancy filled her 20-odd sample vials and Carol left with them immediately. Nancy then started me on two IV medicines: a preventative anti-nausea drug and an antibiotic. It took about 20 minutes for these to drip into my body.
Next up was my first "real" chemo drug, Cytoxan. The Stanford V protocol used to use Nitrogen Mustard, a very nasty drug that started out as a chemical warfare weapon in WWI. Amazingly, Mustard also can be used to cure cancer, but has many undesirable side effects. In the last few years, the Stanford protocol has been revised to allow the use of Cytoxan instead if desired or if the Mustard is not available (as was the case for my visit). This was good news to my ears, as I had been very concerned about the use of Mustard.
The Cytoxan took 30 minutes to drip into me, and then Nancy injected the next two medicines by hand. She used a huge horse-sized needle, but since she was injecting into my IV line, it didn't affect me any differently. If I had received this injection in my arm, the smaller veins there would have definitely felt it -- the cold for sure, and maybe some burning from the medicine. The huge veins in my chest weren't affected in the least by the injection. The portacath is 2-0!
The first injected medicine, Adriamycin is red in color and can be very deadly to your body, causing heart damage or even death. I think this is why they inject it by hand under the nurse's close supervision. The whole injection process only took 2-3 minutes. An interesting side effect of this drug is that my urine turned red/orange for the next few times I used the bathroom. [Update, 19 November: I used to have a cool picture of me peeing orange, but too many folks complained so I took it down... you can see it here if you want :-).]
The final drug of the day was Velban, which injected quickly also. This drug can cause constipation (not a joking matter, as it can kill you if ignored) and numbness or tingling in the hands and feet. I am supposed to tell the doctor if I feel either of these systems, although the tingling is a side affect that sometimes lasts for months after treatment ends.
We wrapped things up with a final saline drip to flush out my portacath and provide a bit of hydration for me. Nancy then handed me my new patient binder, which is an awesome collection of all the information I need for my entire treatment. It contains emergency contact phone numbers, a list of the drugs I'm on, eating tips and recipes, how to cope with side effects, data sheets for tracking my treatment received and my blood levels. They put a lot of work into this thing; it's probably a solid 100 pages and is going to take a few days to digest.
I wrapped things up by scheduling my second treatment, same bat time, same bat place, exactly one week in the future. My treatment next week will use totally different medicines than the ones I received this week. As you may have seen if you have read up on Stanford V, the treatment alternates medicines on even and odd weeks to provide intense treatment in half the time of conventional treatment. I'll have a full explanation of those drugs and their side effects after my next visit.
So how was my chemo office visit? Much better than I expected. I didn't experience any pain at all, nor any sickness or discomfort. The people were friendly and the office was pleasant. It basically felt like sitting in a La-Z-Boy for a couple of hours with an IV sticking into me. I felt much worse after my two recent surgeries than I felt after chemotherapy.
But... the effects are sure to come. To prepare for this, I was given 6 prescriptions to fill (which Aimee graciously did for me after dropping me off at the BOOM! Condo to lie down):
- Kytril: First line of defense against nausea and vomiting. Taken twice a day for two days following each chemotherapy treatment.
- Prochlorperazine: Prevents any nausea that the Kytril doesn't get. Taken every 6 hours as needed.
- Ativan (aka Lorazepam): Also prevents nausea, but primarily relieves anxiety and causes drowsiness. Taken as needed before bedtime to help me sleep.
- Pepcid (aka Famotidine): Prevents ulcers and stomach problems. Taken twice a day.
- Bactrim DS (aka SMZ/TMP DS): Antibiotics to prevent infection. Taken every Monday, Wednesday, and Friday.
- Prednisone: This steroid is actually part of the Stanford V regimen and not just a side effect drug. Steroids fight cancer directly, although I'm not sure how that works. One side effect of Prednisone is that it will help keep my energy level up. I have to take 70mg every other day for 9 weeks. The pill only comes in a 10mg size, so I have to take 7 pills each time. This is so many pills (225 in all) that the pharmacy ran out and we have to go back tomorrow to get the rest of the order.
The pharmacist saw all the drugs we were getting and threw in a free pill minder. I don't think I can use it, though, because the scheduling is so difficult on all of these drugs. I think a two pill minder system (AM and PM) might work.
Aimee filled in a nice calendar to help me keep track of what to take when. (You may need to be a member of my Yahoo! group to view this. If you aren't a member, see the "Mailing List" section at the top-right of this page.)
As the evening draws to a close, I am definitely starting to feel the effects of having 9+ drugs coursing through my body. The battle within has begun. I don't feel sick per-se, just a funny feeling in my head, but I definitely wouldn't be up for doing much of anything right now. Let's hope I can get a good night's sleep tonight.
- 10 November 2003, Monday -- Trial assignment; worry
-
Tomorrow is my first day of chemotherapy. I had an exciting "Chemo's Eve" preparing for it.
First, a woman named Chris called me from Dr. Karamlou's office and told me that she was going to be my patient advocate. She is available as an additional resource if I have questions about anything. She was quite knowledgeable about insurance and billing issues, and I was able to get some good information from her that I'll use to select my health care coverage at work for 2004.
Around 3:00, the clinical trials nurse, Carol Purdy, called me and asked if I could come downtown right away for a chest x-ray and a uric acid blood test. These tests were necessary to complete the prerequisites for my entry into the trial. I learned that she had been frantically working to get everything done before the end of the day. The trial has very strict rules about how old records can be when they accept patients, and my first CAT scan from 4 weeks ago was going to expire and become invalid at the end of the day!
Luckily, Carol's dedication is without rival. She worked until almost 7:00 to get everything in order. Some last minute jitters reared their ugly heads and I started to question whether I should be doing the trial at all. Carol tracked down Dr. Karamlou and even the pharmacist at the hospital and assuaged my fears. I had to admire her skill and resourcefulness at navigating the health care system and getting fast results after hours. She truly wanted me to be fully informed so that I could be comfortable with my decision.
I provided some last minute data to her over the phone, which she entered into the trial web site while I waited, and in only a few minutes, I knew which randomized group I had been assigned to. And the survey says...
Stanford V!
Now, after weeks of worrying about which treatment is better for me, I get to worry about whether I made the right decision. I think worry is the very essence of the cancer patient's plight. Worry before treatment about what to do. Worry about how your life is going to change. Worry during treatment that it's not working. Worry after treatment, while waiting for the test results, that you might not be not cured. Worry for the rest of your life that it might come back.
And it is thus that I don't know whether to be ecstatic or scared that I'm doing the Stanford V treatment. I know that Stanford is the world leader in Hodgkin's research, and that the treatment has shown significantly higher success rates in patients with my risk profile. But then that nagging doubt sets in... Of course, if I had been assigned to the ABVD group, I would be typing a list of reasons I'm worried about it instead!
I'm very anxious (and a little scared) about how things are going to go tomorrow. All along, I have heard that everybody reacts to chemotherapy differently. Over the next few days, I will learn what the next three months of my life are going to be like. I can already tell that I'm not going to get a very good night's sleep tonight.
- 7 November 2003, Friday -- Final pre-treatment meeting with Dr. Karamlou
-
I took the surgical dressings off my chest last night and was amazed to see that there wasn't a trace of blood on the bandages. Dr. Khaki did a really good job of suturing me up. I'm still pretty sore, but rapidly getting better. The catheter protrudes about 1/4" from my chest (you can barely make it out in the pictures, just below the bandage strips). The area is still swollen from surgery, so I expect the catheter to become less pronounced, although I suspect it will always be visible since I have such low body fat.
I had my final pre-treatment meeting with Dr. Karamlou today, after which I decided to enter the clinical trial. I will find out by Tuesday whether I was randomly assigned to the ABVD or Stanford V arm of the trial. Here's how I got to this decision:
After meeting with Dr. Segal, I had pretty much decided on the Stanford V treatment, to the point that I was going to demand it outside of the context of the trial. Something that is often confusing to people is that the Stanford V treatment itself is not a clinical trial. Both ABVD and Stanford V are FDA-approved regimens that can be administered by any doctor. The clinical trial I am entering is trying to decide whether Stanford V is more effective than ABVD. The trial is being conducted by the Southwest Oncology Group in coordination with the National Cancer Institute and the Columbia River Oncology Program. I found this technical overview on the web very informative, or you can read the trial consent form for a layperson's version.
However, after meeting with Dr. Nichols and doing some more research on my own, I got really freaked out about the mandatory radiation that comes with Stanford V and flip flopped to wanting ABVD treatment. Some of the side effects from radiation (such as having my thyroid gland destroyed, increased risk of secondary cancer, and losing my voice) sounded extremely unappealing to me. Radiation treatment is also given every weekday for an entire month, which is going to be really inconvenient.
So I entered the meeting with Dr. Karamlou with the sole purpose of discussing this radiation issue. I knew that ABVD treatment also requires follow-up radiation in cases of "massive mediastinal disease". Since the majority of my disease is in my mediastinum, I was worried that this might include me. Luckily, "massive" means greater than 1/3 the width of the chest; since mine is only 7.5cm wide, I am considered "bulky" instead. While this is good news, it doesn't rule out possible radiation under ABVD therapy. Dr. Karamlou predicted that I would have a 50% chance of requiring radiation even after 6 cycles (24 weeks) of ABVD. After the chemotherapy is complete, a PET scan would determine whether I would need the radiation or not.
This revelation completely invalidated the reasoning that had led me to ABVD. After losing sleep all week worrying about whether to take ABVD or Stanford V, I have finally come to the conclusion that I am splitting hairs here. They are both good treatments, with their respective pros and cons: ABVD is time-tested, but longer and may require radiation. Stanford is much shorter, but requires radiation and is not as mature as ABVD. Either way, my chances are really good, probably the best that a cancer patient can hope for. (Also, Dr. Karamlou agreed to substitute a more modern drug, Cyclophosphamide, in place of Nitrogen Mustard if I end up with Stanford V. Since Nitrogen Mustard is a really nasty drug that, among other things, causes sterility, this eased my mind considerably.)
So, I decided to let fate decide my treatment and entered the trial. I'll get the better medical care that comes from participating in a trial and get to help society and advance science as well. As Dr. Nichols said in his "obligation of the cured" speech to Lance Armstrong after his recovery from cancer:
"Anyone cured in the year 2002 has a great debt to the patients that have gone before him. I believe if you're given such a great gift in terms of being returned to health from such a dreaded disease, you need to remember that and make sure that in some ways you serve future generations with the same sort of illnesses."
- 6 November 2003, Thursday -- Second sperm bank visit
-
I was home today recovering from the port catheter surgery, so I figured I would take advantage of the time and make a second trip to the sperm bank downtown. I probably should have just stayed home and taken it easy, but "doubling up" of medical tasks has become de rigueur for me of late. I start feeling restless if I'm not doing something related to my treatment at all times. I am looking forward to starting chemotherapy so I can slow down and focus solely on one thing (getting better) rather than the myriad tasks I'm juggling right now.
My previous journal entry on the trip to the fertility clinic resulted in a torrent of e-mail feedback, so I took my camera down there this time to satiate the appetite of the ravenous readers out there. These pictures show the collection chair, the lockable chest with the well thumbed through literature, the sink, and the secret door that you put the sample in when you're done.
My first collection produced enough sperm for 3 storage vials (I'm still trying to get the exact sperm count and motility from the report). Each vial can be used for one IUI (intrauterine insemination) attempt, which has a 25% probability of resulting in a pregnancy. The IUI is the preferred approach since it is cheap (around $100); the alternative is in vitro fertilization, which is very expensive (>$10,000 per attempt).
On my last visit, there was a box of unused collection cups next to the chair. Before coming today, I had decided to take an extra cup home with me and just do the "sample collection" there rather than at the clinic (the clinic is only a 5 minute drive from my condo). I didn't see the box this time, so I rummaged around beneath the sink looking for it. I did indeed find it, along with the "special reserve" collection of literature. We're talking some hard core stuff here. I take it that they reserve this stuff when sample collection isn't working with the normal material. [Update 8 November: By popular demand, here is a list of the magazine titles that I remember from under the sink: Hustler, Club, Gallery, 18, Barely Legal, Playgirl (I guess it makes sense that gay men give samples too), and a Victoria's Secret catalog (seemed strangely out of place in there).]
Each additional sample collection costs $65, if you were wondering. When you go into the room, the door locks automatically behind you, and a giant light goes on above the door to let you know that it's safe to proceed. When you're done, you just get up and leave. The staff seem to avoid eye contact, and nobody speaks unless you speak to them first.
[Update, 18 November: Finally found out my sperm counts: 103 million sperm per mL, motiliy 35%. I believe the motility number is post-thaw.]
- 4 November 2003 -- Central venous catheter surgery
-
We arrived at the hospital a few minutes early for my 2:30 check-in time. The woman at the desk said, "we've been looking for you!" Apparently they moved up my surgery time from 4:30 to 3:30 and didn't bother to tell me! Having just been through here two weeks before, there wasn't much paperwork to fill out and I was used to the drill. It wasn't long before I was in my hospital gown and laying in my assigned pre-op room.
The nurses this time seemed much more sassy than previously and I had a good time with them. I mentioned I was cold, and they immediately brought some warm blankets right out of the dryer for me, and then refreshed them a couple of times over the next hour or so with new warm blankets. It was good.
The nurse asked why I was in here since I looked so healthy. This happens to me all the time (usually from people at work or strangers). It doesn't offend me, but it does make for an awkward period where the person tries to figure out what to say. Often people start relating to you some story about how somebody they know had cancer and is doing fine now. I also get eyeballed all the time from people at the doctors' offices; I can sense that they are wondering why I'm there. (Most doctors' offices I've been in are the exclusive province of the very young or the very old.)
The surgeon, Dr. Khaki, stopped by for a quick pre-op chat and I showed him the CAT scans that I had brought with me. The pathology report had said that the lymphoma had enveloped the great vessels in my chest, and I wanted to make sure that he knew what he was getting into. He said no problem, he would try to put the port on the left side, but could go over to the right side if necessary. As this incident demonstrates, I have become very proactive in my health; I view the doctor as a partner in my medical treatment and I never assume that he knows everything.
The anesthesiologist, Dr. Wong, stopped by also. I liked his bedside manner a lot more than my previous anesthesiologist. In addition, unlike the previous guy, Dr. Wong had called me the night before to see if I had any last minute questions, which was really cool. Based on my consultation with the surgeon the previous week, I had thought that I would be getting general anesthesia, but Dr. Wong said sedation was fine (I agreed, since it means a much quicker recovery time). Unlike last time, I didn't get any drugs until I got into the operating room.
In response to my repeated questions, the nurses told me that the drug used for conscious sedation is called Versed. With this drug, you stay awake through the entire procedure and are able to answer questions, follow commands, and even move. But the drug erases your memory of the whole thing so you remember nothing. (Isn't is scary what they can do with medicine?) Last time, the doctor started me on Versed in my pre-op room, and I only remember a few fragments of the whole operation.
This time, I got to experience everything: Meeting with the operating room nurse, who wheeled me down to the OR by herself. Passing through the large, metal, freezer-like door of the OR (complete with big freezer-like handle). Moving myself onto the OR table. Looking up into the alien-looking OR lights. Having an oxygen tube inserted into my nose. Having a blood pressure cuff and fingertip heart rate/oxygen saturation gizmo put on. Dr. Khaki's shaving my chest with an electric razor.
The OR is not a very comfortable room to be in. I was feeling very nervous at this point and could feel bile or something equally unpleasant pooling in my throat. I thought I might actually throw up, which seemed impossible since I hadn't eaten since 8am that morning. I didn't have to panic for long as Dr. Wong injected the Versed into my IV... the last thing I remember was listening to a rhythmic "beep... beep... beep" echoing throughout the room. I am pretty sure it was my heart rate, and it felt good to know that I was the center of attention, that all of these people were here for the express purpose of helping me.
Fast forward an hour (which I don't remember), and I "woke up" in the recovery room. I recovered much more quickly than before. I think it's because Dr. Wong was a better anesthesiologist and used the bare minimum drugs necessary for the operation. Last time, I had to be wheeled out in a wheelchair, and I almost blacked out on the way home. This time I was able to walk out myself, and we even went to a restaurant and ordered take-out for dinner. - 4 November 2003, Tuesday -- Dr. Nichols (third opinion)
-
Aimee and I were very excited to finally meet the much heralded Craig Nichols, who is famous for treating Lance Armstrong's testicular cancer. He also specializes in Hodgkin's Disease. We have been waiting over two weeks to meet with him, which may not sound like a lot of time for most things, but when you have cancer, it's an eternity.
My first impression of the OHSU oncology office is that it was bustling with activity. The first two offices we visited were lethargic by comparison. I guess when you have world renowned doctors on the premises, everybody shows up to see the oracle.
I used the rest room while waiting for the doctor, and passed by the chemotherapy treatment area. It was like a scene out of a science fiction movie: Ten or so people reclined back in dentist-like chairs with high-tech-looking pumps delivering the chemo drugs through IVs in their arms. The room curved around, much like that scene at the beginning of 2001 when the astronaut is jogging around the space ship. What made the scene eerie was the utterly sterile feel of the room, the gentle puffing of all the IV pumps in the quiet room, and the fact that everybody was just sitting with their eyes closed, each in his/her own world. This contrasted tremendously to the "chemo area" of Dr. Karamlou's office, which comprised comfy La-Z-Boys and (while I was there) plentiful Halloween decorations to cheer things up.
We weren't waiting all that long when a very young doctor walked in the room. He introduced himself as Dr. Something-Hyphenated, currently in his fellowship at OHSU under Dr. Nichols. He proceeded to run through the collection of my medical history, which I have grown accustomed to after visiting with Drs. Karamlou and Segal. He then left to consult with Dr. Nichols and upload his data dump.
Soon thereafter, Dr. Nichols entered the room, sat down, and immediately got down to business (Dr. Something-Hyphenated sat in the corner observing). Since the data gathering was out of the way, I proceeded with my questions, pretty much the same ones I asked Dr. Segal:
- Do you agree with my staging? He said, yes - I am well into stage 3.
- Should I get a flu shot/Pneumovax? Not a bad idea, but I am too close to starting chemo now.
- How many new Hodgkin's patients do you see a year? 2-3 a month! (Versus 2-3 per year with the other doctors.)
- What do you think about Drs. Karamlou and Segal, and how would you recommend choosing a doctor? He said Dr. Karamlou trained under him and he has "every confidence" in him. He was rather enigmatic about Dr. Segal and said simply, "he used to be on the faculty here at OHSU". He said the most important part of the process in treating Hodgkin's is choosing the treatment. Once that has started, any competent doctor can administer the protocol. He offered to do "tag team" treatment, with Dr. Karamlou as my primary, but with him checking in periodically.
- Most importantly of all, what treatment do you recommend? As expected, he said ABVD is the most trusted regimen, having treated tens of thousands of people. He said Stanford V was promising, but has treated less than 1,000 people. He said that he would only endorse Stanford V as part of the clinical trial. I mentioned the German treatment BEACOPP, and he said that it was a very tough protocol and way more treatment than I needed given my risk factors.
Somewhere during the questioning, I paused to collect my thoughts, and Dr. Nichols stood up and started to leave. I definitely wasn't done asking questions, but managed to squeeze a few more during an awkward period while we were all standing up. I know he's an expert in Hodgkin's and has many patients to see, but I felt like I needed more time.
Aimee's and my overall grade for our visit with Dr. Nichols was only average, compared to an A for Dr. Karamlou and an A+ for Dr. Segal. Maybe he felt that it was just a second opinion so it didn't need as much time, but I definitely do not feel like I had an adequate visit with Dr. Nichols. Of course, he is the best there is when it comes to Hodgkin's -- when you go to the source, it's intense, but you only get a short time. I still think Dr. Nichols is an A+ doctor, but for whatever reason the office visit just didn't go as well as the others. [Update 6 November: I talked to Dr. Karamlou and he said that Dr. Nichols called him and discussed working tag team. This buoyed my spirits since I get the best of both worlds now: Personalized care from Dr. Karamlou with occasional checkpoints with a Hodgkin's expert. Looking back, I wonder if Dr. Nichols ended our meeting quickly since he had already decided that working tag-team with Dr. Karamlou would be the best solution.]
Unfortunately, my third opinion meeting with Dr. Nichols did not bring the closure I was seeking with respect to which treatment I should take. He was not bubbling over with enthusiasm about Stanford V, and he agreed with some research that Dr. Segal had mentioned that has proven that radiation treatment does not make a difference in success rate in patients whose tumors are less than 1/3 of the width of their chest (as is the case with me -- my tumors are 7.5cm wide at the largest point).
We went home and immediately hit the net for some more research. I found several Hodgkin's support groups that were a wealth of information. Most notable to me was that I couldn't find anybody who has been treated with Stanford V since 1999-2000 time frame. If it's such a good protocol, then why hasn't everybody switched over to it? I did find a lot of stories about people who had suffered nasty side effects from radiation. It's true that chemotherapy is no walk in the park, but the permanent side effects seem less bad than with the radiation. Many of the people on the support groups expressed that the chemo had not been that bad and they were able to lead pretty normal lives most of the time.
So I don't know where that leaves me, except that I need to pick something and start treatment really soon. I have more or less decided to go with Dr. Karamlou. I have the best rapport with him, and Dr. Nichols has agreed to "tag team" treat me with him. I have another meeting on Friday to discuss the pros and cons of radiation therapy versus just sticking with good old fashioned chemo.
- 3 November 2003, Monday -- Sperm bank
-
I went down to University Fertility
Consultants, signed some paperwork, and forked over $300. This initial
payment covers the first collection, some testing they have to do, and one year
of storage. Additional collections are $65 each time. They won't know until
after the testing how many "samples" have to be collected to ensure a
reasonable chance of pregnancy down the road. For most men, apparently, two
samples are sufficient per child. Everybody at the fertility office uses the
word "sample" to avoid any awkwardness.
Samples are run through various diagnostic tests and processing and then put into 1.8mL vials. Each vial contains 20 million sperm. The vials are then stored in liquid nitrogen at -196 degrees C. This thwarts my plans to save money on the storage fee by using my freezer at home.
The place was deserted when I got there, but had several anxious looking people waiting in the lobby when I left. More so than most medical offices, the fertility clinic struck me as the place where people's greatest wishes come true, but also where utter helplessness and futility are realized much of the time.
After paying, the woman led me back to the "sample collection room", which was much more clinical than I was expecting. I had envisioned a comfy La-Z-Boy chair in a warm and inviting setting, but was greeted by your standard tiny medical room with vinyl coated chairs. I was left in the room with a cup and not much in the way of instructions. Another way to avoid embarrassment, I suppose.
There was a little wooden chest with a lock on it. Inside were half a dozen Penthouse, the literature of choice for sample collection it seems. The chest had a little lock on the side, and I chuckled to myself as I imagined the staff locking things down at night for maximum security.
I'll find out my sperm count in a day or two, after which I'll know how many times I have to go back. I plan on banking enough to have two kids. This seems sufficient as the whole thing is only a precautionary measure anyway.
- 31 October 2003, Friday -- Second opinion; Dr. Segal
- Aimee and I saw Dr. Segal at Northwest Cancer Specialists for my
second opinion today. NCS and OHOA (where my first doctor is) are the
two biggest private cancer groups in Portland. Dr. Segal is definitely
a very caring doctor, and also very precise and thorough. After talking
for about an hour, he said "you seem like a really nice guy, I'm
sorry this had to happen to you." And he personally escorted us out to
the main entrance when we were done. I thought that was nice. He also uses
very precise medical terms and talks through his thought process out loud,
which my engineering mind appreciates. At one point, he said, "Engineer, eh?
I feel for you; the analytical minds of engineers often struggle the worst with
trying to choose treatment".
For the most part, Dr. Segal corroborated what Dr. Karamlou said. He did disagree with some of the pathology findings from my CAT scans, especially the one concerning my chest. None of these minor discrepancies really matter, because the end result is the same: Advanced stage 3B lymphoma, requiring long treatment (6-8 cycles of chemotherapy). He said there is really no difference in treatment between stage 2 and 3 anyway; it only really matters that I'm not stage 4. Normally, he would have done a PET scan as well, but again, it really wouldn't change my treatment at this point, so he sees no need. He did strongly recommend a post-treatment PET scan to ensure that I am completely cured.
One significant departure from Dr. Karamlou is that Dr. Segal thought I should get both a flu shot and a Pneumovax vaccination.
He did mention a new German treatment BEACOPP that has a 5-year survival rate of 91 percent. He said if I lived in Europe, I would probably be on this regimen "no questions asked", but the US medical community was not sold on it yet vis-a-vis ABVD.
He walked me through some research that had been shown to predict a patient's 5-year survival rate after ABVD treatment based on 7 factors. You start with a 5-year survival rate of 82% and then subtract 5% for each factor that you have. The factors are: Being male. Being anemic. Being stage 4. Having a high white blood cell count. Being older than 45. Having a low lymph count. And having an albumin count less than 4.
I only have one indicator (being male), so my predicted 5-year survival rate by this method is 77% (for ABVD therapy). Yikes. That's getting a little low for comfort.
Like Dr. Karamlou, he mentioned the ABVD/Stanford V trial and recommended it. I asked him bluntly if Stanford V wasn't clearly the better regimen. He agreed that it has been around a long time and seems to increase survival rate percentages an additional 5-10% above the ABVD numbers above.
I then mentioned my worries about joining the trial and randomly being assigned to the control group (ABVD) and not getting the Stanford V treatment. I told him that I struggle internally with my desire to help society and advance science versus my internal drive to do what's best for me, no matter what. I asked if he would give me Stanford V treatment outside of the trial. He started to say "no, you should join the trial", but then debated with himself out loud, and then surprised me by saying, "you obviously have done a lot of thorough research, and if you tell me that you want Stanford V, I'll give you Stanford V."
We then asked him about the difference in care between different oncologists, and how we should choose between him, Dr. Karamlou, and a doctor like Craig Nichols who is a Hodgkin's expert. (Dr. Segal sees about 2 Hodgkin's patients a year.) He told us that he felt that the medical care would be the same anywhere, but "if you want to see the guy that sees the most Hodgkin's patients, Craig Nichols is the guy." (He said that the vast majority of his patients do not get a second opinion, despite his recommendation to do so. We both found that amazing.)
One concern I've heard about OHSU (where Craig Nichols works) is that it has a clinical feel to it due to the large academic presence -- never seeing the same nurse twice, lots of different doctors on fellowship, etc. People that have gone to OHOA or NCS find them more personal. But the quality of the care should be good either way.
There were a lot of kids in the waiting room at NCS, something I haven't seen before. I wonder if they specialize in pediatric oncology. It's very sad to think of little kids with cancer. And on Halloween to boot.
- 30 October 2003, Thursday -- MUGA scan; CAT scan pathology
-
I had my MUGA
scan at Good Samaritan today. First, the technician drew 5cc of my blood
which was then mixed with a radioactive isotype. After waiting 30 minutes for
the mixture to settle, my blood was injected back into me, which gave me the
willies big time. I then lay down inside the scanner for two separate scans.
The radiation level of the mixture is quite low, so each scan takes 10 minutes,
during which you cannot move the area being scanned. The camera (basically a
huge metal plate) must be positioned very close to your body; I didn't have any
problems, but I could easily see how one could feel claustrophobic in there.
This all took place in the "nuclear medicine" area of the hospital. I think it's called nuclear medicine because the radiation is inside the body emitting outward, whereas with regular radiology (x-rays/CAT scans/etc.), the radiation starts outside and is sent through the body.
All of this is done to measure the ejection fraction of my heart, or how much blood is expelled from the left ventricle of my heart with each beat. A normal LVEF is 50%; have to wait and see what mine ends up being... [Update, 31 October: Dr. Segal told me my LVEF is 65%.]
Before the MUGA scan, I had a brief stop at Dr. Khaki's office to discuss the catheter surgery. We scheduled it for next Tuesday afternoon, under general anesthesia.
Yesterday, I called up the CAT scan place and asked them to give me my neck and chest CAT scan records. In the findings, they mention a "1.5cm left jugulodiagastric node" (that's the one I knew about on my neck) and a 5cm by 2.5cm node near the thyroid gland. That's the one that was pushing against my esophagus... I had no idea it was so freakin' big! The node extends down into the chest all the way to the carina (which, thanks to Google, I now know is about 30cm below the teeth) and has a maximum diameter of 7.5cm. [Update, 1 November: A doctor friend told me that the carina is where the trachea splits into two parts, one each for the left and right lungs.]
Yowsers, that's big! I definitely feel like it's time to get started on the treatment. It seems like one of the nodes on my right neck is starting to get big too... the clock is ticking.
I scanned in the neck/chest and abdomen/pelvis pathology reports.
- 29 October 2003, Wednesday -- Pulmonary function test; first bill
-
I went to Good Samaritan hospital today for my pulmonary function test. For
this test, I sat inside an airtight chamber and did various types of breathing
through a tube in my mouth: deep inhaling, deep exhaling, panting, holding
breath, etc. The end result is a baseline of my current (healthy) lung
condition that can be used as a reference point during treatment to ensure that
the chemo isn't damaging my lungs. The computer used to record the results was
surprisingly low-tech, basically an old beat-up PC running Windows 95 with some
shareware-looking software, but whatever gets the job done!
Relative to the average for my demographic group, my lung capacity scores were disappointingly low, about 85% of reference. On the bright side, my lungs are 30% more efficient than average, so I guess it balances out. Looks like I won't be taking on Lance Armstrong anytime soon... [Update, 1 November: A doctor friend wrote me and commented that my decreased lung capacity is probably the result of the enlarged lymph nodes in my chest compressing my trachea.]
The bill from my neck surgery/biopsy came today. Aye-yah! $6500. I just can't believe such a short, simple operation was so expensive. I had written earlier that the whole hospital experience was "like flying first class". Well, it's as expensive as first class too! Interestingly, the lab and pathology work was almost 50% of the cost.
If you had asked me earlier to guess how much the total treatment cost is going to be (including everything), I would have said $15,000. I'm going to upgrade that to $50,000 now. Aimee's vote is $100,000. Send me your guess and we'll see who's closest in the end.
I also read the informed consent form for the Stanford V trial. The form details all of the risks and benefits of joining a clinical chemotherapy trial. It contained tons of information about the side effects of the drugs, which was a little sobering, but also reassuring because the really nasty long-term side affects seem to be rare (less than 2% occurrence).
- 28 October 2003, Tuesday -- Staging; Dr. Karamlou; discuss all test results
-
I met with Dr. Karamlou again today to discuss all of my test results.
The bone marrow biopsy came back normal. All of the bloodwork came
back normal, including my sed rate.
This means that the disease has not spread to my blood or bone marrow yet.
The abdomen and pelvis CAT scan revealed a single abnormal 2.5cm lymph node behind my pancreas (this is in addition to the known infected nodes in my chest and neck). The maximum size that a healthy lymph node should be is 1.0cm. Because this lymph node is below my diaphragm, this news pushes me into stage 3 Hodgkin's disease. This means that I will need to take the long cycle of chemo, whereas stage 1 or 2 patients can consider a short cycle. There is a possibility that the lymph node is enlarged for some other reason; a PET scan would reveal whether the node is cancerous or not, but rather than look for other causes, Dr. Karamlou feels that it is probably the Hodgkin's spreading. Being a strong believer in Occam's Razor, I can't help but agree.
I am still eligible for the clinical trial comparing ABVD to Stanford V. Previously, I had thought that you could just sign up Stanford V and get in, but there is a randomization step involved. Half of the trial participants are control subjects and get the traditional ABVD treatment. The other half get the new Stanford V treatment. The drugs are basically the same in either case; the Stanford protocol tweaks the levels of the drugs received each week, is administered in 12 weeks (versus 24 weeks for ABVD), and uses localized radiation to remove any large tumors that remain. The basic idea with the Stanford protocol is to use as little chemo as possible to avoid causing medical problems down the road. Because the ABVD treatment lasts longer and kills more of the tumors, radiation is often not needed afterwards.
One advantage of being in the trial is that post-treatment care is much more thorough. For example, trial participants get routine CAT scans after treatment is complete, whereas non-trial patients would not usually do this. And, of course, participating in the trial contributes to the advancement of medicine. Unlike early drug trials (where the drug company pays all of the costs), you have to pay all of the expenses (or I should say, your insurance company).
I have to get two more diagnostic tests and one more surgery before treatment can begin. Hopefully this will be the end of the tests and surgeries!
- A MUGA Scan to assess the overall health of my heart. One of the drugs used in chemo (Adriamycin) can be toxic to the heart and this test ensures that my heart is strong enough to allow the use of that drug. This is an out-patient procedure that takes a couple of hours.
- A pulmonary function test. Another drug used in treating Hodgkin's is Bleomycin, which can cause lung damage. This test provides a baseline that can be compared against in treatment to make sure the Bleomycin is not doing any damage to my lungs. This is an out-patient procedure that takes about an hour.
- Surgery to implant a central venous catheter. This is a semi-permanent device placed underneath the skin above my left breast (it comes out after treatment is complete). It allows me to receive IV treatments and to give blood samples without having to get poked in the arm every time. It is also necessary because the drugs used in chemotherapy are so strong that they will damage the smaller veins in the arms normally used for injecting medicine. The catheter allows direct access to one of the largest veins in the chest, which will not be affected by chemo. This implant requires a surgeon (I'll be going back to Dr. Khaki) and requires a half-day stay in the hospital. (Does anybody else remember that movie Dune where they had the planet where everybody had to have a "heart plug" installed. If the emperor didn't like you, he would yank out your heart plug and you would bleed to death. I feel like I'm getting one of those installed in me...)
Dr. Karamlou still seems very interested in treating me and recommends joining the clinical trial. I still need to get the second opinions from the other doctors, after which I can make up my mind. Dr. Karamlou asked me to call him and let him know either way when I had decided. This part of the process made me feel a little awkward and sad, like having to break up with a girlfriend. He's a nice guy and I hope his feelings won't be hurt if I decide to go with another doctor for treatment. I honestly haven't made up my mind yet, but I can sense pressure from Aimee and others to go with one of the other doctors, who are a lot older than Dr. Karamlou.
I also met with Carol Purdy, a clinical trials nurse. She gave me a lengthy disclaimer/consent form that needs to be signed before I can join any trial. If I join the trial, she would be part of my treatment (an "extra set of eyes monitoring you" as she put it), in addition to the regular treatment that I would receive from Dr. Karamlou's office. This is one example of the more thorough treatment that trial participants receive.
- 26 October 2003, Sunday -- Weekend of waiting
-
It's been a pretty uneventful weekend, basically just killing time
until the test results are back in and I find out just how sick I really
am. All of this is quite ironic as I feel quite healthy (although I did
have one more night sweat the other night); the only pain I'm in is the
direct result of diagnostic tests or surgeries: the lymph node biopsy
from my neck (almost 100% healed now) and the bone marrow biopsy (still
a little stiff).
The other irony is that the only way to get rid of lymphoma is to take an otherwise healthy body, inject caustic chemotherapy drugs, and kill off just enough cells, but not too many, to get rid of the cancer and make sure it doesn't come back. I know that doing nothing would be a death sentence as the cancer would be allowed to multiply unchecked, but it's still daunting to think that in a couple of weeks' time I'll be feeling sick.
My biggest concern right now is trying to figure out which oncologist to go with for my treatment. Maybe the decision will be obvious after I meet them all, but since I have nothing else to worry about until the test results are back, I worry about this. During the bone marrow biopsy, Dr. Karamlou mentioned that there is some disagreement in the medical community about how to handle stage 2A/2B patients that are on the cusp between minor cases of the disease and much more advanced cases. Stanford researchers advocate a less-toxic chemo regimen for the less severe cases. Since I am pretty sure I am going to be stage 2A/B, I think this means that I may have some tough choises to make. Things will definitely be easier if all three doctors recommend the same treatment.
- 23 October 2003, Thursday -- Bone marrow biopsy; abdomen and pelvis CAT scan
-
Day of tests. Started off with a bone marrow biopsy at Dr. Karamlou's
office. This is an out-patient operation done under local anesthesia that
involves poking a big needle into your pelvic bone (near the small of your back)
and extracting 5cc of bone marrow. The marrow is bright red and has a more
watery consistency than blood. He also cut off a small piece of bone (approx.
3/4" long by 1/8" wide) that will be used for a biopsy.
I had heard that bone marrow extraction is a horribly painful operation, which didn't turn out to be the case, but it was definitely the most painful thing I've done so far as a result of this whole Hodgkin's thing. The sucking out of the marrow itself caused a preternatural, unescapable pain that felt... well, like somebody sucking the soul out of your bones! I envisioned the marrow desperately holding on before being sucked up into the needle.
The second part, the breaking off the small piece of bone for the biopsy, was by far the most painful part of the procedure. It felt like the anesthesia wasn't even working at that point. I retreated into some karate deep breathing exercises to manage the pain until things were done. Luckily, the whole procedure start-to-finish only took about 10 minutes, and the bone removing part was only about a minute. A dull ache remained afterwards, but not bad enough to require any pain killers.
I then went over to Body Imaging for the abdomen and pelvis CAT scan. I was given a fairly large bottle (450mL) of liquid agent to drink before the scan. The agent makes the organs and vessels stand out more clearly when they are bombarded with the X-rays. The agent was milky white, cold, and not bad-testing, sort of like a chalky, watered-down smoothie. They also injected me with a dye. The scan itself was pretty quick: One time through the machine in under 20 seconds. The head CAT scan that I had had earlier was 4-5 scans from different angles. I talked the technician into letting me see the results of the scan, which are displayed on a high performance computer workstation. Each scan is a narrow slice of your body; you control which slice you are seeing with a slider bar next to the picture. She zoomed all along my body pointing out my heart, lungs, kidneys, liver, major arteries, and intestines. Pretty damn cool. It would be fun to have one of these babies to play around with at home, although the radiation would probably catch up with you :-)
I'm starting to feel a bit like a lab rat getting poked and prodded all the time. Some statistics so far:
- Had 8 visits to various offices and labs (each time having to tender my insurance card -- can't we computerize/standardize/centralize some of this stuff?!)
- Been poked 6 times (3 bloodwork + 3 IVs)
- Had 2 surgeries, removing from my body: lymph node; bone marrow; bone fragment; blood
- 2 new scars on my body (neck and lower back) from aforementioned surgeries
- Been injected with: Unknown "MAC" anesthesia drugs; local anesthesia; dye markers for CAT scan
- Been prescribed: Oxycodone (for pain after neck surgery). [Update 4 November: Apparently this is some pretty strong stuff. When I went back for my catheter surgery, I told them that the Oxycodone didn't really work on me the first time and could I have something else. They said that Oxycodone was the strongest stuff out there!]
- 22 October 2003, Wednesday -- Dr. Karamlou; Diagnosis
- I met with Dr. Karamlou today. He confirmed that I definitely
have Hodgkin's Disease (actually pretty easy to diagnose due to the
presence of the Reed-Sternberg cell). After a brief
exam, his initial thought is that I am stage 2B (see these staging pictures).
I need to have a few more tests to finish the diagnosis (called "staging" because it determines the extent of the disease):
- HIV test (routine test they give to all lymphoma patients)
- Blood tests: LDH and tumor marker tests
- Abdomen and pelvis CAT scan (to see how many lymph nodes have been affected)
- Bone marrow biopsy (to see if the disease has spread to my bone marrow).
Once the test results are back, we can discuss treatment options, which basically boil down to: chemotherapy (if it isn't too far spread) or chemotherapy and radiation (if it is more advanced).
We discussed the following two treatment options for chemotherapy:
- ABVD, a tried-and-true chemotherapy cocktail consisting of 4 anti-cancer drugs. The drugs are administered every 2 weeks for about 6 months. ABVD has been proven effective and is not as damaging to the body as previous therapies (sterility is still a significant risk however, and sperm banking is recommended).
- Stanford V Protocol, a new therapy that alternates high and low doses of different cocktails over a shorter period of time. The side effects are supposed to be much lower with Stanford V and it has a six-year survival rate of 93%, although it is not as widely proven or tested as ABVD. Dr. Karamlou's opinion right now is that this is the preferred treatment. He feels that trials are more regimented and have better follow-up care.
I'm scheduled for the bone marrow biopsy and abdomen/pelvis CAT scan tomorrow. All the results should be back by next week. I have a follow-up appointment scheduled to discuss the results next Tuesday.
On the bright side, he said I can pretty much do whatever I want: Exercise as hard as I want. Party as hard as I want. Take whatever medications (i.e., Flonase, since my allergies seem to be acting up) or pain killers that I want.
- 21 October 2003, Tuesday -- Trying to find an oncologist
- Still trying to get in to see some doctors. Aimee and I have compiled a
short list of doctors that we want to see:
- Frederick Ey (recommended by my primary care physician),
- Craig Nichols (treated Lance Armstrong's testicular cancer and specializes in Hodgkin's)
- Bruce Dana (recommended by an oncologist friend of Aimee's dad).
- Gerald Segal
Unfortunately, these guys are all booked up solid until November and/or on vacation! I need action now, before this thing gets any worse! Very frustrating. The scheduling people at Oregon Hematology Oncology Associates (now part of Knight Cancer Institute) are pretty empathetic to my case, however, and squeeze me onto Kasra Karamlou's schedule. He works in the same office as Dr. Ey (OHOA, one of the two "biggie" cancer organizations in Portland).
- 20 October 2003, Monday -- Neck biopsy results
- After a long weekend waiting, biopsy results are finally back. Dr. Khaki
is in London for an emergency, but Dr. Doshi's office gets the results. They
confirm Dr. Doshi's earlier suspicion that I have lymphoma, specifically
Hodgkin's. They refer me to an oncologist for further treatment.
When I call the oncologist's office, the earliest they can see me is 2 weeks away. Aye-yah! I call back Dr. Doshi's office and they try to expedite things for me. For my peace of mind, I want to get into the office as soon as possible so I can find out how bad it is and what's going to happen to me.
I've been doing some research on the Internet and Cancer.gov and think I might have either stage 2A or 3A Hodgkin's.
- 15 October 2003, Wednesday -- Neck biopsy surgery
-
The surgery went fine, although it was definitely more involved than I was
expecting. I thought it was going to be a
stick-a-needle-in-your-neck-and-get-a-sample type of affair, but it was the
full-on surgery with the IV drip, my butt hanging out the back of a gown, an
anesthesiologist, and nurses rolling me around the hospital on a cart. I don't
really remember the operation, but I do remember waking up in the recovery room
with a sore neck. I thought I was feeling fine, but on the drive home (Aimee
driving, not me :-), my vision started to black out and I had to lie down as
soon as I got home.
After effects of the anesthesia, I'm sure, but I did take the rest of the week off from work as I was prone to losing consciousness
on the pain medication (warning label says "do not drive while taking this
drug").
The entire hospital experience at St. Vincent's exceeded my expectations. It felt like flying first class. I would wholeheartedly recommend having surgery there.
- 14 October 2003, Tuesday -- CAT scan results; Dr. Khaki
- Results from the CAT scan are in. Dr. Doshi calls me in the morning and
says she is concerned that I might have lymphoma. The pressure I feel in my
throat is from an enlarged lymph node pressing against my esophagus. She wants
me to see Dr. Ali Khaki at St. Vincent's Medical Center that same afternoon for
a second opinion and to schedule a biopsy.
Dr. Khaki examines me and says that he doesn't know what I have. He schedules surgery the next day. He is going to remove one of the inflamed lymph nodes from my neck so that it can be analyzed. Apparently this is the only way that they can figure out what's going on. I initially panicked (don't I need my lymph nodes?!) but subsequent research on the Internet reveals that the body has a lot (maybe hundreds) of these smaller "level 3" lymph nodes.
- 13 October 2003, Monday -- Neck and chest CAT scan
- I go in for my CAT scan. Body Imaging is awesome when it comes to scheduling people the same day! The nurse/technician injects a dye intravenously; I can feel the warmth of the dye as it enters my heart and then shoots down my spine/central nervous system. The CAT scanner is a really cool instrument -- quick, painless, and non-invasive.
- 11 October 2003, Saturday -- Ultrasound results
- Dr. Doshi's office surprises me with a weekend phone call, telling me the ultrasound is inconclusive. This comes as no surprise to me given how blurry all those baby ultrasounds always look to me. They want me to go in for a head CAT scan on Monday.
- 10 October 2003, Friday -- Dr. Doshi; Ultrasound
- Dr. Krisciunas is out of the office for a few weeks, so I see Dr. Doshi instead. She says that the neck bump is not normal and suspects a thyroid nodule. She schedules me for an ultrasound later that day at Body Imaging [Update 2012: now known as Epic Imaging]. She is also concerned that I have lost a lot of weight since my last visit (over 10 pounds); I tell her that I just finished a bike trip across the country and I think I may have lost the weight from that.
- 9 October 2003, Thursday -- Second Adam's apple
- While returning from a road trip to Yosemite, I notice a bump at the base of my throat, like a second Adam's apple. The lymph nodes on the left side of my neck are also swollen considerably. I make an appointment to see my primary care physician (Dr. Victor Krisciunas at Sunset Medical Center) the next day.
- September 2003 -- Throat discomfort
- A few weeks before the end of my bicycle trip across America, I start to have the feeling of something caught in my throat (like an aspirin), especially when I lean my head forward or am lying on my stomach. But otherwise feel fine.
- March 2003 -- Hyperthyroidism
- Aimee's relatives think I have buggy eyes and am too skinny. They suspect hyperthyroidism. I get a full physical, including hyperthyroid test, and everything comes back clean. I also have night sweats for a couple of weeks, but they eventually go away on their own. Again, another case of wondering if this was an early symptom. [Update: 22 October: Dr. Karamlou suspects that this was an early symptom of Hodgkin's.]
- January 2003 -- The beginning
- I have an unexplained rash on both legs (ankles and lower legs) and severe itching that keeps me up at nights. Doctor prescribes cortisone cream which seems to take care of the problem. In retrospect, one has to wonder if this was an early symptom...?